| Malignant Melanoma, pigmented
congenital nevus and regression./
Melanoma Maligno, nevus pigmentado congenito
e involucion.
************************************
************************************
****** DATA-MEDICOS **********
************************************
MELANOMA MALIGNO, NEVUS GIGANTE PIGMENTADO E INVOLUCION
MALIGNANT MELANOMA, PIGMENTED CONGENITAL NEVUS AND
REGRESSION
**************************************
****** DERMAGIC-EXPRESS No.49 *******
****** 14 ABRIL DE 1.999 ***********
14 APRIL 1.999
**************************************
***************************************
EDITORIAL ESPAÑOL
=================
Saludos amigos del DERMA-CYBER,,, el tema de hoy MELANOMA MALIGNO, NEVUS GIGANTE PIGMENTADO E INVOLUCION. Pueden realmente estos nevus experimentar regresión espontanea. ??? Revisé la literatura y encontré algunas referencias que apoyan estos comentarios. Espero que las disfruten.
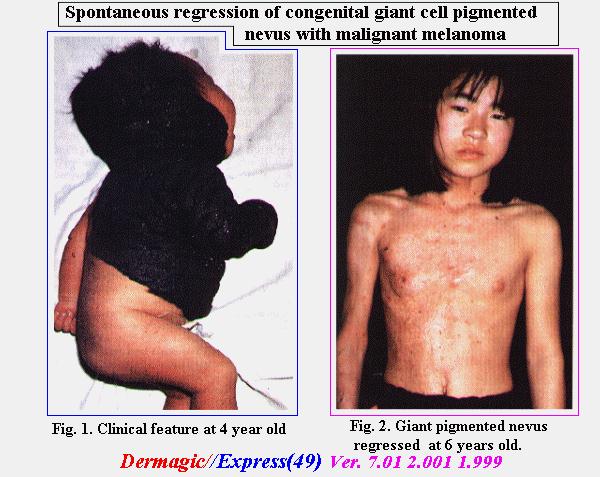
En el attach 1 lamina ilustrativa de la referencia No.1 Spontaneous regression of congenital giant ceil pigmented nevus with malignant melanoma,, ...alguien diria por alli "aunque usted no lo crea..."
Saludos a TODOS !!!
PROXIMA EDICION: LA D-PENICILAMINA , LO BUENO Y LO MALO.
Dr. Jose Lapenta R.,,,
EDITORIAL ENGLISH
=================
Greetings friends of the DERMA-CYBER, today's topic MALIGNANT MELANOMA, PIGMENTED CONGENITAL NEVUS AND REGRESSSION. Really can these nevus to experience spontaneous regression. ???. Look for in the literature and I found some references that support these comments. I hope enjoy them.
In the attach 1 illustrative sheet of the reference No.1) Spontaneous regression of congenital giant cell pigmented nevus with malignant melanoma,,, ...somebody would say... believe it..or not."
Greetings to ALL!!!
NEXT EDITION: THE D-PENICILLAMINE, THE GOOD AND THE BAD.
Greetings to ALL, !!
Dr. Jose Lapenta R.,,,
======================================================================
DERMAGIC/EXPRESS(49)
======================================================================
1.) Spontaneous regression of congenital giant cell pigmented nevus with malignant melanoma (attach file melano.gif)
2.) Pigmentary regression in a giant nevocellular nevus: a case report and a review of the subject.
3.) Spontaneous resolution of a giant congenital melanocytic nevus.
4.) Regressing malignant melanoma.
5.) Spontaneously regressing malignant melanoma with unusual histological features.
6.) Metastatic malignant melanoma with spontaneous and complete regression of the primary lesion. Case report and review of the literature.
7.) The many faces of completely regressed malignant melanoma.
8.) Immune response against human primary malignant melanoma: a distinct cytokine mRNA profile associated with spontaneous regression.
9.) Double choroidal malignant melanoma in an eye with apparent clinical regression.
10.) Effect of IFN-alpha on tumor-infiltrating mononuclear cells and
regressive changes in metastatic malignant melanoma.
11.) Regression of cardiac involvement by malignant melanoma following
lomustine chemotherapy.
12.) Malignant melanoma risk factors by anatomic site: a case-control study and polychotomous logistic regression analysis.
13.) Clonal T cell responses in tumor infiltrating lymphocytes from both regressive and progressive regions of primary human malignant melanoma.
14.) Prognostic factors in thin cutaneous malignant melanoma.
15.) Histologic regression in malignant melanoma: An interobserver concordance study
16.) Histological regression in malignant melanoma: recognition, incidence and significance (Meeting abstract).
17.) Complete spontaneous regression of cutaneous primary malignant melanoma
18.) Lymph nodes with metastatic melanoma of unknown primary site
19.) Malignant melanoma of the parotid gland
========================================================================
=======================================================================
1.) Spontaneous regression of congenital giant cell pigmented nevus with malignant melanoma
=======================================================================
J.-I. Hasegawa, N. Maeda, T. Kanzaki, N. Mizuno
Departments of Dermatology, Nagoya City University Medical School, Nagoya, Japan
case report:
A 13-year-old Japanese girí was seen with a giant pigmented nevus on her right temple, scalp, neck, upper trunk and right arm, present already at birth (Fig 1). This pigmented nevus gradually faded away by casting off black crusts or scales from the surface over a time span of 13 years (Fig. 2). The black lesion totally flattened and became normal in color leaving several small neurofibroma-like nodules (Fig. 2). At the age of 6 years a nodular black pedunculated tumor 3 cm in diameter de-veloped on her upper back. This proved to be a malignant melanoma histologically. The tumor was excised locally. A recur-rence or metastasis has not been observed since then for 7 years.
Histological findings at birth.
Two types of histology were observed. One was a compound nevus with irregular acanthosis and hyperkeratosis, and the other a com-pound nevus with neurofibroma-like der-mis. Both of them showed strong junction-al activity and casting off phenomenon (transepidermal elimination). No cellular atypia was observed.
Histological findings at 6 years of age
(malignant melanoma and nevus).
The malignant melanoma was composed of 2 celí types i. e. spindle and epithelioid celís. The nevus resembled a neurofibroma; there was no junction~ activity what-soever. There are 4 possibilities in the spontaneous regression of nevocellular nevi and malignant melanoma. These are 1) Sutton's phenomenon (4), II) transepi-46 dermal elimination (2), III) neurofibro-matous and IV) fatty degenerations.
Fig. 1. Clinical feature at 4 days oid.
Fig. 2. Giant pigmented nevus regressed at 6 years oíd.
(see the attach)
The spontaneous regression of congeni-tal pigmented nevus of our case is believed to be caused by the transepidermal elimi-nation of nevus celis as reported by Kan-zaki et al. (2).
Many black crusts or scales were sbed from the lesion resulting in clearing of the nevus, as the parents reported. This was supported by the histological examination, which revealed the nevus celís being elimi-nated from the epidermis. The nevus celís in the dermis were replaced by neuro-fibromatous celis in the deeper dermis.
To our best knowledge, tliis is tbe first case which showed complete spontaneous regression of a congenital giant pigmented nevus.
References
1. Copeman PWM, et al. Br J Dermatol 1973; ~ 127
2. Kanzaki T, et al. The l2th International Pigment Ceil Conference. 19~3; p 1(13
=======================================================================
2.) Pigmentary regression in a giant nevocellular nevus: a case report and a review of the subject.
=======================================================================
ARTICLE SOURCE: Pediatr Dermatol (United States), Aug 1988, 5(3) p178-83
AUTHOR(S): Zack LD; Stegmeier O; Solomon LM
PUBLICATION TYPE: JOURNAL ARTICLE; REVIEW (42 references); REVIEW OF REPORTED CASES
ABSTRACT: A giant congenital nevocytic nevus (CNN) on the trunk was followed in a patient from age three months to 23-years-old. During that time the nevus underwent pigmentary regression leaving 2-3 mm lentigines without any evidence of vitiligo or halo formation around the giant CNN. Histopathologically, nevus cells remained in the dermis.
=======================================================================
3.) Spontaneous resolution of a giant congenital melanocytic nevus.
=======================================================================
ARTICLE SOURCE: Pediatr Dermatol (United States), Aug 1988, 5(3) p170-2
AUTHOR(S): Hogan DJ; Murphy F; Bremner RM
PUBLICATION TYPE: JOURNAL ARTICLE
ABSTRACT: This is the second report of a case of spontaneous resolution of a giant congenital melanocytic nevus, which was documented both by photographs and skin biopsies. Cases of spontaneous resolution of these lesions may represent a vigorous host response against an aberrant clone of melanocytes.
=======================================================================
4.) Regressing malignant melanoma.
=======================================================================
Author
Grafton WD
Address
Louisiana State University School of Medicine, Shreveport 71130.
Source
J La State Med Soc, 146(12):535-9 1994 Dec
Abstract
Malignant melanoma may undergo spontaneous regression. This phenomenon
may
cause difficulty in clinical or pathologic diagnosis. The cases
reported in the literature as
complete spontaneous regression of primary malignant melanomas have been
diagnosed only in retrospect, after the patient presented with
metastatic malignant
melanoma. Two cases of malignant melanoma with partial regression are
reported. In
these cases the areas of complete regression cannot be recognized as
malignant
melanoma. The definitive diagnosis of malignant melanoma can be made
only in the
areas with at least two of three characteristic features of melanoma,
(1) melanocytic cells
with atypical nuclei and prominent nucleoli, (2) mitoses in
melanocytic cells, and (3) invasion
of the epidermis by atypical melanocytic cells. Clinical features
suggesting regressing
malignant melanoma include changes in color, especially areas of
depigmentation,
variations in color in different areas of a pigmented mole, and
decrease in size of a mole.
Histopathologic features of regression include loss of melanin pigment
from the epidermis,
melanophages in the dermis, telangiectasia of capillaries in the
dermis, and lymphocytic
infiltration in the dermis in a band-like or perivascular pattern.
These histologic findings may
also be found in inflammatory lesions such as lichen planus and in
regressing benign
melanocytic nevi.
=======================================================================
5.) Spontaneously regressing malignant melanoma with unusual histological features.
=======================================================================
Author
Tamura A; Ishikawa O; Miyachi Y
Address
Department of Dermatology, Gunma University School of Medicine, Japan.
Source
Acta Derm Venereol, 74(6):451-3 1994 Nov
Abstract
An 85-year-old man with spontaneously regressing primary malignant
melanoma is
reported. Histological features were considered to be compatible with
those of
spontaneously regressing malignant melanoma, except that many
multinucleated giant
cells were observed replacing typical melanoma cells.
=======================================================================
6.) Metastatic malignant melanoma with spontaneous and complete regression of the primary lesion. Case report and review of the literature.
=======================================================================
Author
Shai A; Avinoach I; Sagi A
Address
Department of Plastic and Reconstructive Surgery, Soroka University
Hospital, Faculty of
Health Sciences, Ben-Gurion University of the Negev, Beer-Sheva, Israel.
Source
J Dermatol Surg Oncol, 20(5):342-5 1994 May
Abstract
BACKGROUND. Spontaneous regression of malignant melanoma is
characterized by
a partial or complete disappearance of the neoplasm. Partial
regression of melanoma has
been documented in large series, but complete regression is reported
as occurring only
sporadically. OBJECTIVE. To describe a case of metastatic malignant
melanoma
where the primary lesion underwent spontaneous and complete regression
and to review
the literature pertaining to regression of melanoma. METHODS. The
patient was
examined clinically. Wide excision of the skin with the lesion was
performed as well as left
inguinal lymph node dissection. RESULTS. Histologic examination of the
lesion revealed
complete regression of malignant melanoma. Examination of the lymph
node dissected
from the adjacent inguinal area revealed matastatic melanoma.
CONCLUSIONS. Greater
attention should be devoted to identification of regression in
melanoma, clinically and
histologically, evaluating the prognostic implications which
regression might indicate.
=======================================================================
7.) The many faces of completely regressed malignant melanoma.
=======================================================================
Author
Barr RJ
Address
University of California, Irvine, USA.
Source
Pathology (Phila), 2(2):359-70 1994
Abstract
The prognostic significance of clinical and histologic regression of
malignant melanoma
is highly controversial. Although small foci of regression in evolving
malignant
melanomas seem to have little or no effect on morbidity and mortality,
extensive regression
in larger, fully evolved lesions may be associated with poor
prognosis. This chapter
emphasizes the histologic features of regression and the patterns that
are responsible for
diagnostic pitfalls.
=======================================================================
8.) Immune response against human primary malignant melanoma: a distinct cytokine mRNA profile associated with spontaneous regression.
=======================================================================
Author
Wagner SN; Schultewolter T; Wagner C; Briedigkeit L; Becker JC;
Kwasnicka HM;
Goos M
Address
Department of Dermatology, University of Essen, Germany.
Source
Lab Invest, 78(5):541-50 1998 May
Abstract
Spontaneous regression of melanoma lesions is thought to be the result
of an efficient
immune response against melanoma cells in vivo. The outcome of immune
responses is
critically influenced by a complex network of interacting cytokines
present in the local
microenvironment. Analysis of cytokine gene transcription in melanoma
lesions exhibiting
or lacking a sufficient anti-tumor immune response thus may help to
define cytokines or
cytokine combinations critical to the development of this immune
response. In the present
study, we have investigated an extended panel of cytokine and cytokine
receptor genes by
reverse transcription-PCR and in situ hybridization in regressive and
progressive primary
human cutaneous melanoma samples. Whereas the presence of a lymphocyte
infiltrate in
tissue samples was associated with a TH1 cytokine mRNA profile
(TNF-alpha,
INF-gamma, IL12p35, IL12p40, IL2Rbeta, and IL2Rgamma), clinically and
histologically
regressive samples exhibited additionally increased transcript levels
for GM-CSF, IL2, and
IL15. mRNAs of TH2 cytokines IL4 and IL5 were detected only in a minor
portion of
progressive melanoma samples and regressive melanoma lesions. These
results were
further supported by comparison of progressive with regressive regions
in three
melanoma samples. Again, regressive regions contained higher
transcript levels for
GM-CSF, IL2, and IL15. In comparison to cutaneous metastatic melanoma
lesions,
regressive melanomas also overexpressed the same cytokine mRNA
profile. These
results provide evidence for an association of spontaneous regression
with increased
transcript levels for the cytokine combination GM-CSF, IL2, and IL15
in malignant
melanoma. This cytokine combination could be relevant for experimental
anti-tumor
immune response studies and for immunotherapeutic and gene transfer
studies in the
treatment of melanoma patients.
=======================================================================
9.) Double choroidal malignant melanoma in an eye with apparent clinical regression.
=======================================================================
Author
Holck DE; Dutton JJ; Pendergast SD; Klintworth GK
Address
Department of Ophthalmology, Wilford Hall Medical Center, San Antonio,
Texas 78236,
USA.
Source
Surv Ophthalmol, 42(5):441-8 1998 Mar-Apr
Abstract
Multicentric melanomas in the same eye are rare, with few cases
substantiated by
histology and serial sectioning. We report a patient with two
documented choroidal
malignant melanomas in one eye. The initial tumor spontaneously
decreased in size for
over 2 years before a second tumor appeared in a noncontiguous
location in the same eye.
After enucleation, serial sections showed that the two lesions were
independent choroidal
melanomas. We review the literature regarding multiple, independent
intraocular choroidal
malignant melanomas.
=======================================================================
10.) Effect of IFN-alpha on tumor-infiltrating mononuclear cells and
regressive changes in metastatic malignant melanoma.
=======================================================================
Author
H akansson A; Gustafsson B; Krysander L; H akansson L
Address
Department of Oncology, University Hospital, Link¨oping, Sweden.
Source
J Interferon Cytokine Res, 18(1):33-9 1998 Jan
Abstract
Interferon-alpha (INF-alpha) has a documented activity against
metastatic melanoma. To
what extent an antiproliferative effect or tumor cell modulation or
immunomodulation
contributes to this antitumor effect is still uncertain. The role of
immune mechanisms in the
control of malignant melanoma is suggested by several studies.
Therefore, this
investigation used monoclonal antibodies, anti-CD4, anti-CD8, and
anti-CD11c, to study
the occurrence and distribution of tumor-infiltrating mononuclear
cells in 10 untreated and
26 IFN-alpha-treated patients with regional metastatic malignant
melanoma. IFN-alpha
was given for 1-3 weeks before resection of the metastases. The
infiltration of mononuclear
cells in the stroma and close to tumor cells was studied. The duration
of IFN-alpha
treatment was found to be of importance for the immunomodulatory
effect. In patients
treated for < or = 1 week, tumor-infiltrating mononuclear cells were
still mainly localized in
the stroma, similar to the situation in untreated patients. The
differences in CD4+ cells close
to the tumor cells, comparing untreated patients and patients with
various durations of
IFN-alpha treatment, were highly significant (p = 0.009). Thus,
IFN-alpha treatment
resulted in recruitment of CD4+ cells close to the tumor cells.
IFN-alpha had only a weak
effect on the recruitment of CD8+ and CD11c+ mononuclear cells close
to the tumor cells.
Regressive changes in metastases were also analyzed and correlated to
duration of
treatment. Some of the criteria used for histopathologic regression in
primary melanoma
(distorted histologic architecture, low tumor cell density, and
fibrosis) were applied to
analyze the effect of IFN-alpha in metastatic melanoma. The tumor cell
density was found
to be significantly reduced in metastases with marked tumor regression
compared with
metastases with no, or only minor, regressive changes (p < 0.005). A
chi-square analysis
for trend, comparing untreated patients and patients with various
durations of IFN-alpha
treatment, showed that regressive changes of the tumor increased
significantly during
IFN-alpha treatment (p = 0.02).
=======================================================================
11.) Regression of cardiac involvement by malignant melanoma following
lomustine chemotherapy.
=======================================================================
Author
Carpenter MR; Vassallo M; Peat IM; Scriven AJ
Address
Department of Cardiology, Leicester General Hospital, UK.
Source
Postgrad Med J, 73(863):571-2 1997 Sep
Abstract
Cardiac involvement by malignant melanoma is usually a premorbid
event. We present a
case of presumed cardiac involvement by malignant melanoma with
regression
following chemotherapy as demonstrated by transoesophageal
echocardiography.
=======================================================================
12.) Malignant melanoma risk factors by anatomic site: a case-control study and polychotomous logistic regression analysis.
=======================================================================
Author
Chen YT; Dubrow R; Holford TR; Zheng T; Barnhill RL; Fine J; Berwick M
Address
Department of Epidemiology and Public Health, Yale University School
of Medicine, New
Haven, CT 06520-8034, USA.
Source
Int J Cancer, 67(5):636-43 1996 Sep 4
Abstract
This population-based case-control study systematically examined
reported malignant
melanoma risk factors by anatomic site. Study subjects consisted of
548 invasive
melanoma cases diagnosed in Connecticut during 1987-1989 and 494
randomly selected
controls. Multivariate polychotomous logistic regression was used to
determine whether
risk factors differed across anatomic sites. Risk factors examined
included demographic
and pigmentary characteristics, sun exposure-related factors, anatomic
site-specific
sunburn, recreational water activity clothing habits and number of
nevi. A pattern of
site-specificity was observed for sunburn. A history of sunburn at an
anatomic site was
specifically related to the development of malignant melanoma at that
site more so than
at other sites. This site-specificity was consistent with a direct
role for intense, intermittent
sun exposure in the development of melanoma. Age and gender were the
only risk factors
that differed significantly in effect across anatomic sites. The age
difference was explained
by differences in histologic subtype across sites. The gender
difference could not be
explained by sex differences in anatomic site-specific sunburns or in
recreational water
activity clothing habits. Alternative explanations include sex
differences in behavioral
patterns of sun exposure that we did not measure and as yet
unelucidated differences in
susceptibility to melanoma according to sex and anatomic site.
=======================================================================
13.) Clonal T cell responses in tumor infiltrating lymphocytes from both regressive and progressive regions of primary human malignant melanoma.
=======================================================================
Author
thor Straten P; Becker JC; Seremet T; Br¨ocker EB; Zeuthen J
Address
Department of Tumor Cell Biology, Division of Cancer Biology, Danish
Cancer Society,
Copenhagen, Denmark.
Source
J Clin Invest, 98(2):279-84 1996 Jul 15
Abstract
The T cell receptor (TCR) BV variable (V) gene repertoire of tumor
infiltrating lymphocytes
(TIL) found in progressive and regressive regions of the same primary
human melanomas
were characterized by reverse transcription coupled polymerase chain
reaction (RT-PCR).
After surgery, the tumors were divided into different parts which were
judged as regressive
or progressive regions by visual inspection. Subsequently this
diagnosis was confirmed by
histology. From a total of four primary melanomas analyzed, 2 were
drawn to be
HLA-A2+. Only relatively few BV-gene families were expressed at
significant levels in
each of the samples. Comparison of the BV-expression in regressive
versus progressive
regions of the same tumor revealed major differences in all cases
examined. Direct
sequencing of RT-PCR products indicated that highly expressed BV-gene
families were of
clonal origin in both the regressive and progressive regions.
Together, these data strongly
suggest the occurrence of clonal T cell responses in both regressive
and progressive areas
of the same primary tumor. The differences in expression of certain
BV-genes may
correlate with the functional activity of certain populations of
tumor-infiltrating T cells.
Complete regression of primary cutaneous malignant melanoma.
Author
Menzies SW; McCarthy WH
Address
Department of Surgery, Sydney Melanoma Unit, University of Sydney,
Camperdown,
Australia.
Source
Arch Surg, 132(5):553-6 1997 May
Abstract
While partial spontaneous histopathological regression is a common
finding in invasive
primary melanoma, proven complete regression is rare, with only 33
cases having been
documented. None of the patients in these reported cases had a biopsy
specimen taken
from the original lesion, which would unequivocally prove the
diagnosis of complete
regressing melanoma. Over 4 years, we saw a 62-year-old white man who
refused
treatment of a biopsy specimen-proved superficial spreading melanoma
(Breslow
thickness, 0.7 mm) that eventually regressed completely. A biopsy
specimen confirmed
complete histopathological regression. There was no clinical evidence
of regional or distant
metastases throughout the 4 years. To our knowledge, this is the first
documented case of a
biopsy specimen-proved primary melanoma completely regressing. We present
sequential photographic documentation and review the literature about
this phenomenon.
While the prevalence of such an event is unknown, evidence is
presented that it may be
more common than previously thought.
=======================================================================
14.) Prognostic factors in thin cutaneous malignant melanoma.
=======================================================================
Author
M ansson-Brahme E; Carstensen J; Erhardt K; Lagerl¨of B; Ringborg U;
Rutqvist LE
Address
Department of Oncology, Radiumhemmet, Karolinska Hospital, Stockholm,
Sweden.
Source
Cancer, 73(9):2324-32 1994 May 1
Abstract
BACKGROUND. Thin melanomas can metastasize and be lethal. The predictive
importance of tumor thickness in thin melanomas and the specific
features identifying the
patients at risk have not been investigated fully. METHODS. Prognostic
factors were
analyzed in 585 patients with clinical Stage I invasive cutaneous
malignant melanoma
with a thickness of less than or equal to 0.8 mm. The patients were
included in a
population-based cancer registry in Stockholm county during 1976-1987.
They constituted
about 64% of all patients with thin melanomas who were diagnosed in
the region during
the study period. Information was available on age, sex, anatomic site
of the tumor,
histologic type of melanoma, level of invasion, tumor thickness, and
tumor regression. In
a Cox regression analysis, the prognostic importance of each factor
was studied. By a
case-control technique with individual matching for the identified
independent predictors of
recurrence, the additional prognostic information given by type and
grade of inflammatory
response, presence of vertical growth phase, mitotic rate/mm2, and
histologic ulceration of
the tumor was assessed. RESULTS. After a median follow-up time of 50
months, recurrent
disease developed in 26 patients (4%). There was no difference in
recurrence rate between
patients treated with narrow (1-2 cm) or wide (5 cm) excision.
Anatomic site, tumor
thickness, level of invasion, and tumor regression were found to be
independent prognostic
factors in the multivariate analysis. In the case-control study, only
grade of inflammatory
reaction added significant prognostic information. No subgroup could
be identified that was
without risk of recurrent disease. CONCLUSIONS. Thin melanomas do not
seem to
constitute a separate form of melanoma, but compose one end of a
continuous spectrum
of biologic behavior.
=======================================================================
15.) Histologic regression in malignant melanoma: An interobserver concordance study
=======================================================================
AU: Kang-S; Barnhill-RL; Mihm-MC Jr; Sober-AJ
SO: J-Cutan-Pathol. 20(2):126-9 1993
PY: 1993
PT: JOURNAL-ARTICLE
AB-A: Histologic evidence for regression as a prognostic indicator in melanoma has shown conflicting results. To assess if melanoma regression is a consistently identifiable histologic feature, an interobserver concordance study was undertaken. Fifty histologic slides of melanoma with Breslow thickness of 1 mm or less were non-randomly selected from the Massachusetts General Hospital Melanoma Registry. The selection was in favor of those with regression present in 44 of 50 slides (88%). Two dermatopathologists working independently evaluated a 2 mm wide bracketed area in each tissue section and then the remainder of the non-bracketed tissue section for regression. Before and after each slide review, the evaluators were required to read criteria for early, intermediate, and late regression explicitly outlined. The overall concordance rate for the presence and absence of regression was 96% (48/50) in the bracketed area and 90% for the outside area. When the group with regression was subdivided into three stages, interobserver agreement fell to 86% for the bracketed, and 66% for the outside area. In at least 30% of cases where regression was detected in the bracketed area, both reviewers observed two or more stages of regression in the remainder of tissue section. Therefore, subdividing the process is impractical and unrealistic. Consistent histologic identification of regression in melanoma requires a simple and systematic approach which should be applied to future studies that include melanoma regression as a prognostic factor. (Abstract from CANCERLIT AND EMBASE)
=======================================================================
16.) Histological regression in malignant melanoma: recognition, incidence and significance (Meeting abstract).
=======================================================================
AU: Blessing-K; McLaren-KM
SO: J-Pathol. 167(Suppl):162A 1992
PY: 1992
PT: MEETING-ABSTRACT
AB-A: The phenomenon of tumor regression presents a potentially dramatic demonstration in favor of a role for host immunity. Although complete regression in melanoma is rare, partial regression is relatively common; however, there is a wide range of reported incidence, most of which can be explained by differences in criteria for definition of the process. The clinical significance of regression in melanoma also remains unresolved. From the Department of Pathology in Aberdeen, 563 cases of primary melanoma (from a 20-yr period) were assessed for the presence of histological regression, in association with the thickness of the lesion, patient sex, anatomical location and clinical outcome. The extent of lesional regression was assessed semiquantitatively. Regression was more commonly found in thin lesions, being seen in 46% of thin (less than 1.5 mm) lesions, 32% of intermediate (1.5-3.0 mm) lesions and 9% of thick (greater than 3.0 mm) lesions. However, severe regression was only identified in 6.5% of thin lesions, 5.2% of intermediate lesions and 1.5% of thick melanomas. Regression was more common in superficial spreading melanomas and in lesions from the trunk and lower limb, with it being seen slightly more often in men. Clinical follow-up, although not of statistical significance, suggests that regression in thin lesions is a sinister histological feature, supporting results from other centers. (Abstract from CANCERLIT)
=======================================================================
17.) Complete spontaneous regression of cutaneous primary malignant melanoma
=======================================================================
AU: Bottger-D; Dowden-RV; Kay-PP
SO: PLAST-RECONSTR-SURG. 89/3 (548-553) 1992
PY: 1992
PT: Journal-Article
AB-A: Melanomas may first present as nodal metastasis. Most of these cases have a discernible primary source. A proportion of these, however, have no apparent primary. A very few patients in this latter group actually have an identifiable primary source that regressed and disappeared. There is a set of stringent clinical and histologic criteria that must be met before a melanoma can be classified as complete spontaneous regression, and only 24 cases in the literature meet all these criteria. This report reviews those cases and presents the first report to provide sequential photographic documentation of a complete spontaneous regression of a cutaneous malignant melanoma. It also gives a 10-year follow-up, the longest in the literature. (Abstract from EMBASE)
=======================================================================
18.) Lymph nodes with metastatic melanoma of unknown primary site
=======================================================================
AU: Nguyen-T; Avril-MF; Charpentier-P; Guillaume-C; Margulis-A; Prade-M
SO: Bull-Cancer-Paris. 79(3):291-6 1992
PY: 1992
PT: JOURNAL-ARTICLE; REVIEW; REVIEW,-MULTICASE
AB-A: Sixteen patients with clinical stage II melanoma of unknown primary site (regional lymph node metastasis) were followed up between 1978 and 1988. The 5-year survival rate was 47%. These results seem to parallel those for stage II disease with known primary tumor sites, as has been observed in other data from the literature. The hypotheses put forward to explain such lesions are the spontaneous regression of the primary tumor, and the onset of primary malignant melanoma in the lymph nodes. (30 Refs) (Abstract from CANCERLIT AND EMBASE)
=======================================================================
19.) Malignant melanoma of the parotid gland
=======================================================================
AU: Roberts-C; Jayaramachandran-S
SO: Br-J-Clin-Pract. 46(3):217-8 1992
PY: 1992
PT: JOURNAL-ARTICLE
AB-A: We report a case which demonstrates pitfalls in the management of a parotid gland s and highlights behaviour of malignant melanoma that is not widely appreciated. The danger of assuming a benign histological diagnosis of such a mass and the subsequent delay of definitive surgery is demonstrated. Metastases within the parotid gland are not uncommon, melanoma being one of the commonest sources. A search should always be made for a primary tumour in the head, neck and chest. This can be made exceptionally difficult by the uncommon phenomenon of spontaneous regression of the primary melanoma. (Abstract from CANCERLIT AND EMBASE)
======================================================================
DATA-MEDICOS/DERMAGIC-EXPRESS No (49) 14/04/99 DR. JOSE LAPENTA R.
======================================================================
|

