| Discoid Lupus
Erythematous./ Lupus eritematoso discoideo. ************************************
************************************
****** DATA-MEDICOS **********
************************************
LUPUS ERITEMATOSO DISCOIDEO
DISCOID LUPUS ERYTTHEMATOSUS
**************************************
****** DERMAGIC-EXPRESS No.52 *******
****** 05 MAYO DE 1.999 ***********
05 MAY 1.999
**************************************
***************************************
EDITORIAL ESPAÑOL
=================
Hola amigos de la red, DERMAGIC de nuevo con ustedes,,, el tema de hoy,,,
LUPUS ERITEMATOSO DISCOIDEO, patologia interesante por el simple hecho, que
puede permanecer como tal durante muchos años (crónico), o ser el comienzo
o anuncio de otras enfermedades como el lupus sistemico. Espero que estas
61 referencias sean bastante ilustrativas.
En el attach una lámina ilustrativa del tema. Lupus discoideo crónico
en cara, oreja, hombro y cuero cabelludo.
Saludos a TODOS !!!
PROXIMAS EDICIONES: * DERMATOMIOSITIS.
* ESCLEROSIS SISTEMICA PROGRESIVA,
* LUPUS ERITEMATOSO SISTEMICO
(todas antes del 22/05/99) ...si puedo ok
Dr. Jose Lapenta R.,,,
EDITORIAL ENGLISH
=================
Hello friends of the net, DERMAGIC again with you, today's topic, DISCOID
LUPUS ERYTTHEMATOSUS, interesting pathology for the simple fact that can
remain as such during many years (chronic), or to be the beginning or
announcement of other illnesses like the systemic lupus. I hope these 61
references will be quite illustrative.
In the attach an illustrative sheet of the topic: Discoid lupus
Erythematosus chronicus: face, ear, shoulder and scalp.
NEXT EDITIONS: * DERMATOMYOSITIS.
* SYSTEMIC SCLEROSIS (SCLERODERMA)
* SYSTEMIC LUPUS ERYTHEMATOSUS
(all before 22/05/99) If I can...ok)
Greetings to ALL, !!
Dr. Jose Lapenta R.,,,
=====================================================================
DERMAGIC/EXPRESS(52)
=====================================================================
LUPUS ERITEMATOSO DISCOIDEO / DISCOID LUPUS ERYTTHEMATOSUS
=====================================================================
===================================================================
1.) [Treatment of discoid lupus erythematosus with sulfasalazine: 11 cases]
2.) Serologic and clinical features of patients with discoid lupus
erythematosus: relationship of antibodies to single-stranded
deoxyribonucleic acid and of other antinuclear antibody subsets to clinical
manifestations.
3.) An unusual ocular manifestation of discoid lupus erythematosus.
4.) Immunohistochemical detection of proliferation and differentiation in
discoid lupus erythematosus.
5.) Squamous cell carcinoma of the skin in black patients with discoid lupus
erythematosus.
6.) The expression of C3b receptors in the differentiation of discoid lupus
erythematosus and systemic lupus erythematosus.
7.) [Successful treatment of chronic discoid lupus erythematosus with argon
laser]
8.) Discoid lupus erythematosus presenting as asymmetric posterior
blepharitis.
9.) Squamous-cell carcinoma of the scalp arising in lesions of discoid lupus
erythematosus.
10.) Resistant discoid lupus erythematosus of palms and soles: successful
treatment with azathioprine.
11.) Autoantibodies to evolutionarily conserved epitopes of enolase in a
patient
with discoid lupus erythematosus.
12.) Keratin and involucrin expression in discoid lupus erythematosus and
lichen
planus.
13.) Defective degradation of bacterial DNA by phagocytes from patients with
systemic and discoid lupus erythematosus.
14.) [Comparative immunofluorescence study of actinic keratosis and chronic
discoid lupus erythematosus]
15.) Vitronectin colocalizes with Ig deposits and C9 neoantigen in discoid
lupus
erythematosus and dermatitis herpetiformis, but not in bullous pemphigoid.
16.) A comparison of the dermal lymphoid infiltrates in discoid lupus
erythematosus and Jessner's lymphocytic infiltrate of the skin using the
monoclonal antibody Leu 8.
17.) T-cell subsets in lesions of systemic and discoid lupus erythematosus.
18.) A comparative immunohistochemical study of lichen planus and discoid
lupus erythematosus.
19.) Enhanced normal tissue response to radiation in a patient with discoid
lupus erythematosus.
20.) Retinitis pigmentosa and discoid lupus erythematosus.
21.) Discoid lupus keratitis.
22.) Acetylator polymorphism in discoid lupus erythematosus.
23.) Hereditary deficiency of C5 in association with discoid lupus
erythematosus.
24.) Squamous cell carcinoma of the lip developing in discoid lupus
erythematosus.
25.) [Oral discoid lupus erythematosus. Diagnostic considerations apropos of a
case]
26.) Markers in cutaneous lupus erythematosus indicating systemic
involvement. A
multicenter study on 296 patients.
27.) NAT2 genotyping and efficacy of sulfasalazine in patients with
chronic discoid
lupus erythematosus.
28.) ARA and EADV criteria for classification of systemic lupus
erythematosus in
patients with cutaneous lupus erythematosus.
29.) Chronic discoid lupus erythematosus in Thailand: direct
immunofluorescence study.
Kulthanan K; Roongphiboolsopit P; Chanjanakijskul S; Kullavanijaya P
30.) Chronic discoid lupus erythematosus: an immunopathological and
electron microscopic study.
31.) Squamous cell carcinoma of the lip developing in discoid lupus
erythematosus.
32.) Childhood discoid lupus erythematosus.
34.) Systemic sclerosis (scleroderma) associated with discoid lupus
erythematosus.
36.) Clinical, histologic, and immunofluorescent distinctions between
subacute cutaneous lupus erythematosus and discoid lupus erythematosus.
37.) Scarring alopecia in discoid lupus erythematosus.
39.) Chilblain lupus erythematosus: report of 15 cases [see comments]
40.) Sweat gland abnormalities in lichenoid dermatosis.
41.) The progressive systemic sclerosis/systemic lupus overlap: an unusual
clinical progression.
42.) Safety and efficacy of a broad-spectrum sunscreen in patients with
discoid or subacute cutaneous lupus erythematosus.
43.) Hereditary deficiency of C5 in association with discoid lupus
erythematosus.
44.) Response of discoid and subacute cutaneous lupus erythematosus to
recombinant interferon alpha 2a.
45.) Recombinant interferon alpha 2a is effective in the treatment of
discoid and subacute cutaneous lupus erythematosus.
46.) Experimental reproduction of skin lesions in lupus erythematosus by
UVA and UVB radiation [see comments]
47.) Histopathologic comparison of the subsets of lupus erythematosus [see
comments]
48.) Chronic cutaneous lupus erythematosus.
49.) Rowell's syndrome. Report of a case.
50.) Expression of lymphocyte activation markers in benign cutaneous T cell
infiltrates. Discoid lupus erythematosus versus lichen ruber planus.
51.) [Congenital ischemic onychodystrophy (Iso-Kikuchi syndrome) and
chronic lupus
52.) Evaluation of lymphocyte activation in skin lesions of patients with
mixed connective tissue disease and discoid lupus erythematodes.
53.) Autofluorescence of clofazimine in discoid lupus erythematosus.
54.) A family survey of lupus erythematosus. 1. Heritability.
55.) A comparison of the dermal lymphoid infiltrates in discoid lupus
erythematosus and Jessner's lymphocytic infiltrate of the skin using the
monoclonal antibody Leu 8.
56.) Lupus profundus in children: treatment with hydroxychloroquine.
57.) The reliability of immunofluorescence and histopathology in the
diagnosis of discoid lupus erythematosus and lichen planus.
58.) Immunopathology of cutaneous human lupus erythematosus defined by
murine monoclonal antibodies.
59.) HLA genotypes in a family with a case of homozygous C2 deficiency and
discoid lupus erythematosus.
60.) Laser treatment of discoid lupus (case report).
61.) Serologic and clinical features of patients with discoid lupus
erythematosus: relationship of antibodies to single-stranded
deoxyribonucleic acid and of other antinuclear antibody subsets to clinical
manifestations.
====================================================================
====================================================================
1.) [Treatment of discoid lupus erythematosus with sulfasalazine: 11 cases]
====================================================================
Author
Delaporte E; Catteau b; Sabbagh N; Gosselin P; Breuillard F; Doutre MS;
Broly F; Piette F; Bergoend H
Address
Service de Dermatologie A, H^opital Claude-Haried, CHRU, Lille.
Source
Ann Dermatol Venereol, 124(2):151-6 1997
Abstract
INTRODUCTION: Antimalaria agents and thalidomide are two reference drugs
for discoid lupus erythematosus. In non-responders or after secondary
resistance or contraindications, there are a number of alternative
therapeutics which are less effective and more toxic. We therefore
conducted an open study in patients with discoid lupus erythematosus
treated with sulfasalazine. PATIENTS AND METHODS: Seven men and four women
(mean age 40 years) with severe discoid lupus erythematosus (mean duration
of disease 14 years) were treated with sulfasalazine (2 g/d). This
treatment was initiated after a previous failure or contraindication of
antimalarial drugs or thalidomide. The acetylation phenotype was predicted
in all patients with N-acetyltransferase 2 genotyping. Genome DNA was
tested for mutations causing an N-acetyltransferase deficiency. Homozygous
individuals or those with heterozygous composites for the tested mutations
were predicted slow acetylators and those with a homozygous or heterozygous
genotype for an allele carrying a normal sequence at the mutation sites
were predicted rapid acetylators. RESULTS: We had 7 complete responses, 1
partial response and 3 failures. Mean delay to efficacy was 7 weeks, longer
for lesions involving the scalp (4 to 5 months). Six of the 8 responders
were given sulfasalazine exclusively. The effect was suspensive and
dose-dependent; the minimal effective dose was 1.5 g/d. Excepting light
sensitization requiring discontinuation, there were no clinically
significant side effects. Neutropenia occurred in one patient and moderate
and transient live enzyme movements did not require treatment withdrawal.
The only immunoallergic side effect (light sensitization) observed occurred
in a slow acetylator. All responders except one were rapid acetylators.
DISCUSSION: Salazosulfapyridine, or sulfasalazine, is composed of a
derivative of 5-aminosalicylic acid and a sulfamide fraction,
sulfapyridine. It is only marginally used in dermatology except for
psoriasis. Its efficacy in chronic lupus erythematosus has been reported in
one case. We confirmed the role of this compound in the treatment of
chronic lupus erythematosus. The rare observations of induced lupus and
development of antinuclear antibodies are not a contraindication, but
require close regular clinical and biological surveillance. The potential
risk is that possible hypersensitivity could lead to reserving
sulfasalazine for severe resistant chronic lupus erythematosus after
failure with antimalarials and thalidomide. Nevertheless, our study
demonstrates that the slow acetylator phenotype predicts immunoallergic
events, as observed by other authors, and would be a factor predicting
nonresponse. If these results are confirmed by other studies, it would be
possible to propose sulfasalazine as a treatment for discoid lupus
erythematosus in rapid acetylators.
=====================================================================
2.) Serologic and clinical features of patients with discoid lupus
erythematosus: relationship of antibodies to single-stranded
deoxyribonucleic acid and of other antinuclear antibody subsets to clinical
manifestations.
=====================================================================
Author
Callen JP; Fowler JF; Kulick KB
Source
J Am Acad Dermatol, 13(5 Pt 1):748-55 1985 Nov
Abstract
Serologic and clinical data were obtained from forty patients with discoid
lupus erythematosus in 1982. Clinical disease was characterized by quality,
extent, severity, activity, photosensitivity, and systemic manifestations.
The patient's sera were examined for the presence of antinuclear, anti-Ro
and anti-La, anti-ribonucleoprotein and anti-Sm, anti-single-stranded
deoxyribonucleic acid (ssDNA), and antinative DNA antibodies. In late 1984,
thirty-three patients had follow-up clinical examinations. On the initial
evaluation the patients with positive antinuclear antibody (ANA) findings
were clinically characterized by a significantly higher incidence of
photosensitivity and arthritis, an elevated erythrocyte sedimentation rate,
and cutaneous lesions of subacute cutaneous lupus erythematosus. The
activity and extent of disease in 1982 did not correlate with the presence
of ANA. Elevated levels of ssDNA antibodies were present in seven of the
forty patients (significantly greater than control subjects; (p less than
0.005) and correlated with widespread, active discoid lupus erythematosus,
an elevated erythrocyte sedimentation rate, and a slightly greater risk of
systemic lupus erythematosus in 1982. At the 2-year follow-up examination,
thirteen of the seventeen patients with a positive ANA had active clinical
cutaneous disease, and ten of the sixteen patients with negative ANA
findings had continued activity (not statistically significant). However,
all seven patients with elevated ssDNA antibody levels had continued
activity, and disease progression had occurred in three. Thus the presence
of ssDNA seems to correlate strongly with active, progressive lupus
erythematosus. The presence of antibody abnormalities in patients with
discoid lupus erythematosus correlates with clinical disease and provides
more support for the theory linking discoid lupus erythematosus to systemic
lupus erythematosus as part of a continuum.
=====================================================================
3.) An unusual ocular manifestation of discoid lupus erythematosus.
=====================================================================
Author
Foster RE; Lowder CY; Meisler DM; Valenzuela R; McMahon JT; Camisa C
Address
Department of Ophthalmology, Cleveland Clinic Foundation, OH 44195.
Source
Cleve Clin J Med, 61(3):232-7 1994 May-Jun
Abstract
BACKGROUND: Discoid lupus erythematosus is a chronic skin disease
characterized by well-demarcated papules and plaques. Mucous membrane
changes are common; however, conjunctival involvement is unusual. We report
a case of unilateral, chronic, isolated discoid lupus erythematosus of the
conjunctiva. OBSERVATIONS: A 32-year-old man presented for evaluation of
chronic conjunctivitis of the right eye that had persisted for 9 years. A
biopsy of the bulbar conjunctiva revealed a mixed mononuclear cellular
infiltrate distributed along the epithelial basement membrane zone and
around the stromal blood vessels. Immunohistopathologic examination
revealed a diffuse, granular pattern of fluorescence corresponding to
immunoglobulins and complement components along the epithelial basement
membrane zone and in the walls of the stromal blood vessels. Electron
microscopy demonstrated changes in the epithelial basal lamina consistent
with discoid lupus erythematosus, including areas that were multilayered.
Immunoelectron microscopy identified sub-basal lamina deposits of
immunoglobulin G. CONCLUSIONS: Discoid lupus erythematosus should be a
suspected cause of chronic conjunctival inflammation; the diagnosis is
substantiated by immunopathologic and ultrastructural studies.
=====================================================================
4.) Immunohistochemical detection of proliferation and differentiation in
discoid lupus erythematosus.
=====================================================================
Author
de Jong EM; van Erp PE; Ruiter DJ; van de Kerkhof PC
Address
Department of Dermatology, University Hospital Nijmegen, The Netherlands.
Source
J Am Acad Dermatol, 25(6 Pt 1):1032-8 1991 Dec
Abstract
Discoid lupus erythematosus lesions show hyperkeratosis and atrophy, which
may reflect abnormal epidermal proliferation, differentiation, or both. In
this investigation, markers for epidermal proliferation, differentiation
and inflammation were studied in cutaneous lesions of discoid lupus
erythematosus. Frozen sections of biopsy specimens from 20 patients were
examined immunohistochemically regarding Ki-67 staining and keratin 16
expression (parameters for proliferation), and the expression of keratin
10, involucrin, and filaggrin (parameters for differentiation). The
inflammatory infiltrate was characterized with the use of antibodies
against T lymphocytes, monocytes/macrophages, and Langerhans cells. With
these markers, epidermal proliferation was found to be increased in discoid
lupus erythematosus. Keratin 10 expression, a marker for early
differentiation, showed the pattern of normal skin. Involucrin and
filaggrin, markers for terminal differentiation, were expressed already in
the lower part of the stratum spinosum, whereas in normal skin these
markers were restricted to the stratum granulosum and the upper layers of
the stratum spinosum, and the stratum granulosum and stratum corneum,
respectively. Infiltrate analysis revealed the well-established picture. We
conclude that in cutaneous lesions of discoid lupus erythematosus,
hyperproliferation is combined with normal early differentiation and
premature terminal differentiation of keratinocytes.
=====================================================================
5.) Squamous cell carcinoma of the skin in black patients with discoid lupus
erythematosus.
=====================================================================
Author
Caruso WR; Stewart ML; Nanda VK; Quismorio FP Jr
Source
J Rheumatol, 14(1):156-9 1987 Feb
Abstract
Skin cancer is relatively uncommon among black individuals. Squamous cell
carcinoma occurred in a scar of chronic discoid lupus erythematosus in a
black patient. A review of 7 previously reported cases of squamous cell
carcinoma in blacks with chronic discoid lupus erythematosus indicates a
tendency of the cancer to metastasize. Sun exposure of the hypopigmented
lesions of chronic discoid lupus and possibly other factors predispose to
cancer of the skin. Poorly healing skin lesions in chronic discoid lupus
should arouse suspicion of malignant change.
=====================================================================
6.) The expression of C3b receptors in the differentiation of discoid lupus
erythematosus and systemic lupus erythematosus.
=====================================================================
Author
Tausk F; Harpster E; Gigli I
Address
Division of Dermatology, University of California, San Diego School of
Medicine.
Source
Arthritis Rheum, 33(6):888-92 1990 Jun
Abstract
We studied the expression of the C3b receptor, CR1, on erythrocytes (E-CR1)
of patients who, in spite of having mild systemic symptoms, were diagnosed
as having discoid lupus erythematosus and followed accordingly. We found
that E-CR1 was markedly reduced in these patients, similar to that seen in
patients with systemic disease. In contrast, those patients with completely
asymptomatic discoid lupus erythematosus had the same expression of E-CR1
as the normal population.
=====================================================================
7.) [Successful treatment of chronic discoid lupus erythematosus with argon
laser]
=====================================================================
Author
N¨urnberg W; Algermissen B; Hermes B; Henz BM; Kolde G
Address
Hautklinik, Virchow-Klinikum, Humboldt-Universit¨at zu Berlin.
Source
Hautarzt, 47(10):767-70 1996 Oct
Abstract
We report on a patient with chronic discoid lupus erythematosus who was
treated with argon-laser. The patient suffered from long-standing lesions
and had been pretreated with various drugs; with no or slight improvement.
After a few argon-laser applications, the treated skin lesions improved
dramatically while the untreated lesional skin showed continuous disease
activity. Histological and immunohistological investigations of biopsies
from treated and untreated lesional skin suggest that endothelial
mechanisms play a role in the generation and maintenance of discoid lesions
in lupus erythematosus. This is the first reported case of successful
treatment of chronic discoid skin lesions of a lupus erythematosus patient
with argon-laser.
=====================================================================
8.) Discoid lupus erythematosus presenting as asymmetric posterior
blepharitis.
=====================================================================
Author
Gloor P; Kim M; McNiff JM; Wolfley D
Address
Department of Ophthalmology and Visual Science, Yale University School of
Medicine, New Haven, CT 06520-8061, USA. [email protected]
Source
Am J Ophthalmol, 124(5):707-9 1997 Nov
Abstract
PURPOSE: To describe the ophthalmic findings of patients with discoid lupus
erythematosus. METHOD: We describe two women who originally were thought to
have asymmetric posterior blepharitis; however, the involved eyelid also
had an erythematous, scaly cutaneous lesion. RESULT: In both patients,
histology and immunofluorescence studies performed on cutaneous biopsy
specimens established the diagnosis of discoid lupus erythematosus.
CONCLUSIONS: It is important to diagnose discoid lupus of the eyelids
because misdiagnosis can delay treatment and thus lead to deformities of
the eyelid margin. Misdiagnosis can also lead to a complicated
full-thickness eyelid biopsy and delay the diagnosis of systemic lupus
erythematosus.
=====================================================================
9.) Squamous-cell carcinoma of the scalp arising in lesions of discoid lupus
erythematosus.
=====================================================================
Author
Sulica VI; Kao GF
Address
Division of Dermatology, Georgetown University Medical Center, Washington,
D.C.
Source
Am J Dermatopathol, 10(2):137-41 1988 Apr
Abstract
Squamous-cell carcinoma may arise in scars of chronic discoid lupus
erythematosus. Although there have been 19 cases reported previously,
detailed histopathologic features of this entity have not been recorded. We
report a patient with extensive chronic discoid lupus erythematosus
involving the scalp with subsequent development of multiple squamous-cell
carcinomas. The tumors were locally aggressive with recurrences and
invasion into the underlying skull and dura. The patient died of
respiratory failure 4 1/2 years after initial surgical treatment. There was
no clinical evidence of metastasis. Squamous carcinoma arising in discoid
lupus erythematosus can be regarded as a low-grade carcinoma. Although
about 20% of patients developed local recurrences and metastasis developed
in about 30%, fatality occurred in only two patients (10.5%). Pertinent
literature is reviewed, and the histopathologic findings, differential
diagnosis, and biologic behavior of this tumor are discussed.
=====================================================================
10.) Resistant discoid lupus erythematosus of palms and soles: successful
treatment with azathioprine.
=====================================================================
Author
Ashinoff R; Werth VP; Franks AG Jr
Address
Department of Dermatology, New York University Medical Center, NY 10016.
Source
J Am Acad Dermatol, 19(5 Pt 2):961-5 1988 Nov
Abstract
We present the case of two patients with an unusual form of discoid lupus
erythematosus that was confined almost exclusively to the palms and soles.
In both patients this form of discoid lupus erythematosus did not respond
to conventional therapies, which included topical steroids, intralesional
steroids, prednisone, quinacrine hydrochloride, hydroxychloroquine sulfate,
colchicine, and dapsone. Both patients were then treated with azathioprine.
One patient dramatically improved with azathioprine, worsened each time the
azathioprine was stopped or reduced, and responded again to the
reinstitution of therapy. The other patient began taking azathioprine 8
months ago and has also experienced relief of her symptoms. These cases
suggest that discoid lupus erythematosus principally involving the palms
and soles is difficult to treat with conventional medication and that
azathioprine, which appears to be useful, should be tried after the failure
of other therapies.
=====================================================================
11.) Autoantibodies to evolutionarily conserved epitopes of enolase in a
patient
with discoid lupus erythematosus.
=====================================================================
Author
Gitlits VM; Sentry JW; Matthew ML; Smith AI; Toh BH
Address
Department of Pathology and Immunology, Monash Medical School, Prahran,
Victoria, Australia.
Source
Immunology, 92(3):362-8 1997 Nov
Abstract
Although the pathology of discoid lupus erythematosus is well documented
the causative agents are not known. Here, we report the identity of the
target antigen of an autoantibody present in high titre in the serum of a
patient with discoid lupus erythematosus. We have demonstrated that the
antigen is enolase; first, because it has properties consistent with this
glycolytic enzyme (47,000 MW, cytosolic localization and ubiquitous tissue
distribution). Secondly, limited amino acid sequence determination after
trypsin digestion shows identity with alpha-enolase. Finally, the
autoimmune serum immunoblots rabbit and yeast enolase and predominantly one
isoelectric form of enolase (PI approximately 6.1). These results indicate
that the reactive autoepitopes are highly conserved from man to yeast. The
results also suggest that the autoantibodies are most reactive to the
alpha-isoform of enolase, although it is possible that they may also be
reactive with gamma-enolase, and have least reactivity to beta-enolase. The
anti-enolase autoantibodies belong to the immunoglobulin G1 (IgG1) isotype.
This is the first report of IgG1 autoantibodies to evolutionarily conserved
autoepitopes of enolase in the serum of a patient with discoid lupus
erythematosus. Previous reports of autoantibodies to enolase have suggested
associations with autoimmune polyglandular syndrome type I and
cancer-associated retinopathy. This report and an earlier report of what is
likely to be enolase autoantibodies in two patients without systemic
disease suggest that enolase autoantibodies have a broad association and
are not restricted to any particular disease.
=====================================================================
12.) Keratin and involucrin expression in discoid lupus erythematosus and
lichen
planus.
=====================================================================
Author
Ichikawa E; Watanabe S; Takahashi H
Address
Division of Dermatology, Doai Memorial Hospital, Tokyo, Japan.
Source
Arch Dermatol Res, 289(9):519-26 1997 Aug
Abstract
In the present study, keratin and involucrin expression were studied in
cutaneous lesions of discoid lupus erythematosus and lichen planus in order
to gain a better understanding of the abnormal differentiation or
maturation of the epidermal cells in these dermatoses. Ten specimens each
from discoid lupus erythematosus and lichen planus were analyzed by
immunohistochemical techniques, using a panel of monoclonal antikeratin
antibodies and polyclonal anti-involucrin antibody, and five specimens each
were analyzed by one- and two-dimensional gel electrophoresis and
immunoblot analysis using three antikeratin antibodies. No significant
difference was found between the dermatoses. The expression of
differentiation-specific keratins showed a similar pattern to that in
normal epidermis, and involucrin was expressed even in the lower part of
the stratum spinosum. Keratins 6 and 16, which are characteristic markers
of hyperproliferative states, and keratin 17 were detected in
nonhyperproliferative and atrophic epidermis with hydropic degeneration and
inflammatory infiltrates in the dermis. These results suggest that
expression of keratins 6, 16 and 17 in discoid lupus erythematosus and
lichen planus may reflect a wound healing response to the damage to the
basal cell layer, or may be under the control of cytokines produced by
infiltrating inflammatory cells in the dermis.
=====================================================================
13.) Defective degradation of bacterial DNA by phagocytes from patients with
systemic and discoid lupus erythematosus.
=====================================================================
Author
Roberts PJ; Isenberg DA; Segal AW
Address
Department of Haematology, Faculty of Clinical Sciences, University
College, London, UK.
Source
Clin Exp Immunol, 69(1):68-78 1987 Jul
Abstract
The digestion of bacterial DNA by peripheral blood monocytes was impaired
both in patients with systemic lupus erythematosus (SLE) and discoid lupus
erythematosus (DLE). The monocytes of these patients had both a small
quantitative defect in the solubilization of DNA and a marked qualitative
defect in the extent to which this DNA was degraded. In addition,
neutrophils from patients with SLE released significantly less high
molecular-weight DNA than control cells. Digestion of bacterial RNA and
protein by phagocytes was not defective in either disease. The reduced
digestion of DNA by phagocytes resulted in concomitantly larger amounts of
high molecular-weight DNA remaining in these cells. Such sequestration of
DNA may contribute to the persistence of fairly large DNA fragments in the
tissue of patients with lupus erythematosus.
Language
=====================================================================
14.) [Comparative immunofluorescence study of actinic keratosis and chronic
discoid lupus erythematosus]
=====================================================================
Author
Gruschwitz M; Keller J
Address
Dermatologische Universit¨ats-Klinik Erlangen.
Source
Z Hautkr, 62(22):1585-95 1987 Nov 15
Abstract
Regarding systemic (SLE) and chronic discoid lupus erythematosus (CDLE),
the diagnostic value of the lupus band test ist generally accepted. In the
literature, however, there are but few obligatory criteria concerning the
definition of a positive lupus band. In order to illustrate the influence
of sunlight on the evolution of junctional deposits of immunoglobulins, we
examplarily studied actinic keratosis (AK) as a chronic light-dependent
dermatosis. The junctional deposits in AK were qualitatively and
quantitatively compared with the lupus band typical for CDLE. In CDLE we
mostly found more distinct band-like junctional deposits of immunoglobulins
and complements. Light-dependent, non-specific junctional patterns of
immunofluorescence similar to LE, therefore, require clear morphological
criteria of immunohistology.
=====================================================================
15.) Vitronectin colocalizes with Ig deposits and C9 neoantigen in discoid
lupus
erythematosus and dermatitis herpetiformis, but not in bullous pemphigoid.
=====================================================================
Author
Dahlb¨ack K; L¨ofberg H; Dahlb¨ack B
Address
Department of Dermatology, University of Lund, Sweden.
Source
Br J Dermatol, 120(6):725-33 1989 Jun
Abstract
C9 neoantigen immunoreactivity has been found to colocalize with C3
immunoreactivity at the dermal-epidermal junction zone (DEZ) in skin
specimens from patients with bullous pemphigoid, lupus erythematosus and
dermatitis herpetiformis. The present study was designed to elucidate
whether the C9 neoantigen immunoreactivity represents deposition of
membrane attack complexes or non-lytic SC5b-9 complexes. Skin specimens
from 11 patients with pemphigoid, five patients with discoid lupus
erythematosus and from nine patients with dermatitis herpetiformis were
studied with immunofluorescence using both monoclonal and polyclonal
antibodies against C9 neoantigen and against vitronectin (S-protein), an
inhibitor to the membrane attack complex of complement. Specimens from the
pemphigoid patients demonstrated C9 neoantigen reactivity along the DEZ
without detectable colocalized vitronectin. This suggests deposition of
membrane attack complexes in the pemphigoid lesions. Immunoreactivity of
both C9 neoantigen and vitronectin was detected in the DEZ in specimens of
discoid lupus erythematosus and in the tips of dermal papillae in specimens
of dermatitis herpetiformis. The combined presence of C9 neoantigen- and
vitronectin immunoreactivity may indicate deposition of C9 as part of the
non-lytic SC5b-9 complex. The finding reported here of differential
deposition of vitronectin and C9 in different diseases indicates that the
presence of C9 neoantigen immunoreactivity in tissue per se does not
represent the deposition of membrane attack complexes, but that it may also
be C9 deposited as part of the nonlytic SC5b-9 complex.
=====================================================================
16.) A comparison of the dermal lymphoid infiltrates in discoid lupus
erythematosus and Jessner's lymphocytic infiltrate of the skin using the
monoclonal antibody Leu 8.
=====================================================================
Author
Ashworth J; Turbitt M; MacKie R
Source
J Cutan Pathol, 14(4):198-201 1987 Aug
Abstract
Jessners lymphocytic infiltration of the skin (14 cases) and discoid lupus
erythematosus (13 cases) were studied and the lymphoid infiltrates in the
dermis were compared in the two conditions, using a standard
immunoperoxidase technique. Mouse monoclonal antibodies were used to
identify T helper lymphocytes, T suppressor lymphocytes and, using the
antibody Leu 8, "immunoregulatory lymphocytes . It was shown that the
proportions of Leu 8 positive cells was significantly different in the two
conditions. The average percentage of Leu 8 positive lymphocytes in the
dermal infiltrate found in the cases of Jessner's was 65% (range 40-80%)
whereas the average percentage in the cases of discoid LE was 15% (range
2-30%). This observation is further evidence that Jessner's lymphocytic
infiltration and chronic discoid lupus erythematosus should be regarded as
separate entities.
=====================================================================
17.) T-cell subsets in lesions of systemic and discoid lupus erythematosus.
=====================================================================
Author
Kohchiyama A; Oka D; Ueki H
Source
J Cutan Pathol, 12(6):493-9 1985 Dec
Abstract
In 6 patients with untreated systemic lupus erythematosus (SLE) in the
progressive stage, and in 6 with discoid lupus erythematosus (DLE), an
analysis of inflammatory infiltrates was performed in situ using the
avidin-biotin-peroxidase complex (ABC) method with monoclonal antibodies.
In all patients, over 75% of the infiltrates reacted with the pan T-cell
antibody OKT3, but only sporadically with that of B-cell OKB7. In addition,
a large number of the infiltrates were OKIal-positive, indicating that they
were in an activated state. Many OKT8-positive cells were seen infiltrating
the epidermis especially in the vicinity of basal keratinocytes. Staining
for T-cell subsets revealed that the proportion of OKT8-positive cells
(suppressor/cytotoxic) was from 2 to 3 fold higher than that of
OKT4-positive cells (helper/inducer) in lesions of SLE. On the contrary, in
DLE, a predominance of OKT4-positive cells (the OKT4/OKT8 ratio was from
1:1 to 3:1) was observed. Thus, our results provide further evidence that
these 2 main types of LE show quite contrary findings on
immunohistochemical analysis of T-cell subsets, and that besides the
humoral immune mechanism, the cell-mediated immune mechanism may be
involved in the pathogenesis of these disorders.
=====================================================================
18.) A comparative immunohistochemical study of lichen planus and discoid
lupus erythematosus.
=====================================================================
Author
Lee MS; Wilkinson B; Doyle JA; Kossard S
Address
Skin and Cancer Foundation Australia, Darlinghurst, New South Wales,
Australia.
Source
Australas J Dermatol, 37(4):188-92 1996 Nov
Abstract
A comparative immunohistochemical study was performed on skin biopsies from
10 patients with lichen planus and 10 patients with discoid lupus
erythematosus (DLE). A panel of antibodies against T lymphocytes (UCHL-1,
OPD-4, CD8, CD43), B lymphocytes (L-26), granulocytes (Leu-M1), activation
markers (Ki-1, LN-3), macrophages, fibroblasts and dendritic cells (FXIIIa,
S-100, Mac-387, KP-1, vimentin), endothelial cells (CD34), and epithelial
cells (epithelial membrane antigen) was employed using a
peroxidase-anti-peroxidase technique. The recently released CD8 antiserum
required microwave antigen retrieval of formalin-fixed, paraffin-embedded
tissue to label lymphocytes. The results showed many similarities in the
lymphocyte subsets and macrophages between lichen planus and discoid lupus
erythematosus. The most important differences between the two conditions
were statistically significant increases in the number of S-100+ cells in
the epidermis and dermis, FXIIIa+ cells in the dermis and CD34+ vessels
within the inflammatory infiltrate in lichen planus.
=====================================================================
19.) Enhanced normal tissue response to radiation in a patient with discoid
lupus erythematosus.
=====================================================================
Author
Rathmell AJ; Taylor RE
Address
Department of Radiotherapy and Oncology, Cookridge Hospital, Leeds, UK.
Source
Clin Oncol (R Coll Radiol), 4(5):331-2 1992 Sep
Abstract
We report the case of a patient with discoid lupus erythematosus who
developed a severe skin reaction whilst undergoing mantle irradiation for
non-Hodgkin's lymphoma. Widespread moist desquamation occurred after a skin
dose of only 17 Gy and was associated with an abscopal response outside the
treatment area. The case illustrates the need for extreme caution when
administering radiotherapy to patients with discoid or systemic lupus
erythematosus.
=====================================================================
20.) Retinitis pigmentosa and discoid lupus erythematosus.
=====================================================================
Author
Desatnik H; Ashkenazi I; Regenbogen L
Address
Goldschleger Eye Institute, Chaim Sheba Medical Center, Sackler School of
Medicine, Tel-Hashomer, Israel.
Source
Metab Pediatr Syst Ophthalmol, 15(1-3):9-11 1992
Abstract
A 41 year old male is presented who suffers from both advanced retinitis
pigmentosa and active discoid lupus erthematosus. A possible association
between the two pigmenting disorders is discussed as well as the treatment
of the discoid lupus with potentially retinotoxic hydroxychloroquine.
=====================================================================
21.) Discoid lupus keratitis.
=====================================================================
Author
Raizman MB; Baum J
Address
Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Boston
02114.
Source
Arch Ophthalmol, 107(4):545-7 1989 Apr
Abstract
Two patients with long-standing discoid lupus erythematosus developed
acute, unilateral, corneal stromal infiltration and edema. No evidence of
infection was found, and both responded rapidly to topical corticosteroid
therapy. To our knowledge, only one case of stromal keratitis associated
with discoid lupus erythematosus has been published previously. We describe
the first cases, to our knowledge, in which a satisfactory response to
corticosteroid therapy is demonstrated.
=====================================================================
22.) Acetylator polymorphism in discoid lupus erythematosus.
=====================================================================
Author
Ladero JM; Jim´enez LC; Fern´andez MJ; Robledo A
Address
Department of Medicine, Hospital Universitario San Carlos, Facultad de
Medicina, Universidad Complutense, Madrid, Spain.
Source
Eur J Clin Pharmacol, 34(3):307-8 1988
Abstract
Acetylator phenotype was determined, using sulphamethazine, in 37 patients
with histologically confirmed discoid lupus erythematosus, who were free
from visceral damage, and in 157 normal control subjects. Twenty patients
(54%) and 90 control subjects (57.4%) were slow acetylators (p not
significant). Acetylator polymorphism appears not to be related to the risk
of developing pure cutaneous discoid lupus erythematosus.
=====================================================================
23.) Hereditary deficiency of C5 in association with discoid lupus
erythematosus.
=====================================================================
Author
Asghar SS; Venneker GT; van Meegen M; Meinardi MM; Hulsmans RF; de Waal LP
Address
Department of Dermatology, Academic Medical Center, University of
Amsterdam, The Netherlands.
Source
J Am Acad Dermatol, 24(2 Pt 2):376-8 1991 Feb
Abstract
A 29-year-old woman with discoid lupus erythematosus had undetectable
classic pathway complement activity. Hypocomplementemia was due to
selective deficiency of C5. One of her children was also deficient. To our
knowledge this is the first documented case of an association between
discoid lupus erythematosus and C5 deficiency.
=====================================================================
24.) Squamous cell carcinoma of the lip developing in discoid lupus
erythematosus.
=====================================================================
Author
Handlers JP; Abrams AM; Aberle AM; Auyong T; Melrose RJ
Source
Oral Surg Oral Med Oral Pathol, 60(4):382-6 1985 Oct
Abstract
Since the substitution of steroids and antimalarials for irradiation in the
treatment of discoid lupus erythematosus, squamous cell carcinoma arising
in discoid lupus erythematosus is thought by some to be an uncommon
occurrence. A review of the recent literature (subsequent to 1945) revealed
fifteen cases, of which seven occurred in the lips. In one of twelve of the
cases a history of irradiation was documented. In three other cases, there
was no evidence of its use. We report an additional case of squamous cell
carcinoma occurring in the lower lip of a 24-year-old black woman in the
absence of radiation therapy. A review of the literature and a discussion
of possible predisposing factors are presented.
=====================================================================
25.) [Oral discoid lupus erythematosus. Diagnostic considerations apropos of a
case]
=====================================================================
Author
Bermejo Fenoll A; Rom´an Maci´a P; Bag´an Sebasti´an JV; Gonz´alez
L´opez-Briones L
Source
Rev Stomatol Chir Maxillofac, 86(3):156-64 1985
Abstract
The study and presentation of a typical case of discoid lupus erythematosus
with oral lesions in a 30-years old woman, without visceral manifestations
at present, was the motive for a revision and updating of the concepts of
etiology, differential diagnosis, treatment and prognosis of this disease.
The authors emphasize the importance of the clinical and evolving aspect of
the lesions, long-term development, as well as the response to treatment
(an antimalarial synthesis, applied systematically and infiltrates with
betamethasone solution) in order to reach valid diagnostic conclusions. It
is important in the anatomopathological study to include the atrophic zones
of the central portion of the discoid lesion.
=====================================================================
26.) Markers in cutaneous lupus erythematosus indicating systemic
involvement. A
multicenter study on 296 patients.
=====================================================================
Tebbe B; Mansmann U; Wollina U; Auer-Grumbach P; Licht-Mbalyohere A;
Arensmeier M;
Orfanos CE
Department of Dermatology, University Medical Center Benjamin Franklin,
The Free
University of Berlin, Germany.
Acta Derm Venereol (NORWAY) Jul 1997 77 (4) p305-8 ISSN: 0001-5555
Language: ENGLISH
Document Type: JOURNAL ARTICLE; MULTICENTER STUDY
Journal Announcement: 9711
Subfile: INDEX MEDICUS
Lupus erythematosus (LE) is an autoimmune disorder, involving the skin
and/or other
internal organs. As cutaneous variants, chronic discoid LE (CDLE) and
subacute
cutaneous LE (SCLE) usually have a better prognosis, however, involvement
of internal
organs with transition into systemic disease may occur. The aim of this
study was to
assess the significance of some clinical and laboratory criteria that could
serve as
markers for early recognition of systemic involvement in cutaneous LE.
Three hundred
and seventy-nine patients with LE, seen in five cooperating Departments of
Dermatology during the years 1989-1994, were documented by electronic data
processing
according to a common protocol. Two hundred and forty-five of these
patients had
cutaneous LE (CDLE or SCLE), and 51 had systemic LE (SLE) and were included
in this
study. Forty-nine patients with either CDLE/SCLE or SLE were not evaluated
because
of incomplete documentation; also, 34 patients suffered from other LE
subsets and
were likewise excluded from the evaluation. Multivariate statistical
analysis was
used to assess the value of seven selected variables for distinguishing
between the
CDLE/SCLE and SLE groups: ESR, titers of antinuclear antibodies, anti-dsDNA-
antibodies, photosensitivity, presence of arthralgias, recurrent headaches
and signs
of nephropathy. Univariate and multivariate analysis of the obtained data
showed
that signs of nephropathy (proteinuria, hematuria) was the variable with
the highest
statistical relevance for distinguishing between patients with cutaneous
(CDLE/SCLE)
and with systemic LE (SLE) in all statistical models tested, followed by
the presence
of arthralgias and of high ANA titers (> or =1:320). In contrast, low ANA
titers as
well as anti-dsDNA antibodies showed little or no statistical relevance as a
criterion for distinction. It seems, therefore, that cutaneous LE patients
showing
signs of nephropathy, presence of arthralgias and elevated ANA titers (> or
=1:320)
should be carefully monitored, because they may be at risk of developing
systemic LE
involvement.
=====================================================================
27.) NAT2 genotyping and efficacy of sulfasalazine in patients with
chronic discoid
lupus erythematosus.
=====================================================================
Sabbagh N; Delaporte E; Marez D; Lo-Guidice JM; Piette F; Broly F
Laboratoire de Biochimie et Biologie Moleculaire de l'hopital Calmette,
Universitaire de Lille, France.
Pharmacogenetics (ENGLAND) Apr 1997 7 (2) p131-5 ISSN: 0960-314X
Language: ENGLISH
Document Type: JOURNAL ARTICLE
Journal Announcement: 9710
Subfile: INDEX MEDICUS
Sulfasalazine is an effective agent for chronic discoid lupus
erythematosus (CDLE)
but the response to treatment is considerably variable between patients and
is also
unpredictable. The reason for this might relate to differences in
metabolism of the
drug which is extensively acetylated by the polymorphic enzyme
N-acetyltransferase 2
(NAT2). To test this possibility, the N-acetylation phenotype of eleven
patients
with CDLE and treated by standard doses of sulfasalazine was retrospectively
determined by genotyping. A clear-cut difference in the outcome of
treatment was
observed according to whether the patients were slow acetylators (SA) or
rapid
acetylators (RA). Eight out of 11 patients responded to treatment with a
complete or
marked remission of the disease. Seven of them were RA. The three other
patients
who did not respond at all to the drug were SA. In addition, SA seem to be
more
prone to toxic events. These findings strongly suggest that the genetic
polymorphism
of NAT2 is responsible for differences in the response to sulfasalazine in
patients
with CDLE. Therefore, candidates for sulfasalazine therapy should be
genotyped to
identify those patients who might benefit from the drug.
=====================================================================
28.) ARA and EADV criteria for classification of systemic lupus
erythematosus in
patients with cutaneous lupus erythematosus.
=====================================================================
Parodi A; Rebora A
Department of Dermatology, University of Genoa, Italy.
Dermatology (SWITZERLAND) 1997 194 (3) p217-20 ISSN: 1018-8665
Language: ENGLISH
Document Type: JOURNAL ARTICLE
Journal Announcement: 9710
Subfile: INDEX MEDICUS
OBJECTIVE: To verify (1) how many patients with cutaneous lupus
erythematosus (CLE)
fulfill 4 or more American Rheumatism Association (ARA) and European
Academy of
Dermatology and Venereology (EADV) criteria for classification of systemic
lupus
erythematosus (SLE); (2) which criteria are mostly fulfilled; (3) the
severity of the
disease in patients fulfilling criteria; (4) how many patients with systemic
involvement fail to fulfill 4 ARA and EADV criteria. METHODS: We studied 207
patients with chronic and subacute CLE, classified according to ARA and
EADV criteria.
RESULTS: Twenty-four patients with localized discoid (L-DLE; 21.8%), 22 with
disseminated discoid (D-DLE; 30.5%) and 7 with subacute CLE (SCLE; 28%) had
4 or more
ARA criteria. With EADV criteria, these figures fell to 7 (6.4%), 7 (9.7%)
and 6
(24%), respectively. Only 3 L-DLE (2.7%), 5 D-DLE (6.9%) and 3 SCLE cases
(12%)
defined as SLE by ARA criteria and 1, 3 and 3, respectively, by EADV
criteria had a
renal or neurological disorder, hemolytic anemia and/or thrombocytopenia,
vasculitis
or serositis. ARA criteria did not classify 7 patients with a similar
visceral
involvement, while EADV criteria failed in 11 patients. CONCLUSION: In our
patients,
ARA criteria showed a sensitivity of 88%, a specificity of 79%, a positive
predictive
value of 56% and a negative predictive value of 96%. EADV criteria showed a
sensitivity of only 64%, but a specificity of 93%, a positive predictive
value of 61%
and a negative predictive value of 94%. ARA criteria should not be used in
CLE
patients as they are too sensitive, poorly specific and altogether
misleading. EADV
criteria are more specific, but less sensitive.
=====================================================================
29.) Chronic discoid lupus erythematosus in Thailand: direct
immunofluorescence study.
Kulthanan K; Roongphiboolsopit P; Chanjanakijskul S; Kullavanijaya P
=====================================================================
Institute of Dermatology, Bangkok, Thailand.
Int J Dermatol (UNITED STATES) Oct 1996 35 (10) p711-4 ISSN: 0011-9059
Language: ENGLISH
Document Type: JOURNAL ARTICLE
Journal Announcement: 9704
Subfile: INDEX MEDICUS
BACKGROUND: Studies of chronic discoid lupus erythematosus (DLE) lesions
by direct
immunofluorescence (DIF) were heterogeneous with respect to classes of
immunoglobulins and sites where these were deposited. Most of the studies
were done
in the USA and European countries. MATERIALS AND METHODS: To obtain
representative
data from Asiatic countries, we analyzed the direct immunofluorescent
abnormalities
of 100 DLE lesions in Thai patients who were diagnosed on the basis of
clinical and
histologic criteria. RESULTS: Granular deposits at the dermoepidermal
junction (DEJ)
were detected in 90% of cases. The common immunoreactants at the DEJ were
IgG (63%)
and IgM (47%). The deposits were usually combinations of various classes of
immunoglobulins, mostly IgG (53%) and IgM (41%). Deposits of IgG and IgM
alone at
the DEJ were observed in 12% and 8%, respectively. Deposits at colloid
bodies,
dermal blood vessel walls, and epidermal nuclei were sometimes also seen.
CONCLUSIONS: The DIF test of skin biopsy specimens is diagnostically
significant in
chronic DLE. Our study in Thai patients showed that the most common
deposit was a
combination of various classes of immunoglobulins, mostly IgG and often IgM
as well
as C3, and occurred at the DEJ of the involved area.
=====================================================================
30.) Chronic discoid lupus erythematosus: an immunopathological and
electron microscopic study.
=====================================================================
Shahidullah M; Lee YS; Khor CJ; Ratnam KV
National Skin Centre, National University Hospital.
Ann Acad Med Singapore (SINGAPORE) Nov 1995 24 (6) p789-92 ISSN:
0304-4602
Language: ENGLISH
Document Type: JOURNAL ARTICLE
Journal Announcement: 9704
Subfile: INDEX MEDICUS
We studied 100 cases of chronic cutaneous discoid lupus erythematosus
(DLE) to
evaluate the diagnostic sensitivity of immunoreactant deposition and its
possible
role in basement membrane thickening. Histopathology was diagnostic in 71%
of cases.
Sixty-two percent (41/66) of lesions with thickened and 50% (17/34) with
normal
basement membrane had immunoreactant deposition. Ultrastructural study of
6 cases (3
with and 3 without immunoreactant deposition) with thickened basement
membrane all
showed reduplication of the lamina densa. Thickening of the basement
membrane
appears to be contributed mainly by reduplication of the lamina densa
rather than by
immunoreactant deposition. The direct immunofluorescence (DIF) test of
lesional skin
was positive in 58% of patients and was independent of duration of lesion,
age and
sex. Light microscopy has greater diagnostic sensitivity in confirming DLE
lesions
than DIF. Direct salt split skin technique did not increase DIF
sensitivity. Scalp
lesions showed the highest frequency (83%) of immunoreactant deposition.
As C1q was
the commonest immunoreactant found in our study, we suggest that it should be
routinely used when DIF is employed in the evaluation of DLE. DIF is
especially
helpful in confirming cicatricial alopecia due to DLE.
=====================================================================
31.) Squamous cell carcinoma of the lip developing in discoid lupus
erythematosus.
=====================================================================
SO - Oral Surg Oral Med Oral Pathol 1985 Oct;60(4):382-6
AU - Handlers JP; Abrams AM; Aberle AM; Auyong T; Melrose RJ
PT - JOURNAL ARTICLE
AB - Since the substitution of steroids and antimalarials for irradiation
in the treatment of discoid lupus erythematosus, squamous cell carcinoma
arising in discoid lupus erythematosus is thought by some to be an uncommon
occurrence. A review of the recent literature (subsequent to 1945) revealed
fifteen cases, of which seven occurred in the lips. In one of twelve of the
cases a history of irradiation was documented. In three other cases, there
was no evidence of its use. We report an additional case of squamous cell
carcinoma occurring in the lower lip of a 24-year-old black woman in the
absence of radiation therapy. A review of the literature and a discussion
of possible predisposing factors are presented.
=====================================================================
32.) Childhood discoid lupus erythematosus.
=====================================================================
SO - Arch Dermatol 1993 May;129(5):613-7
AU - George PM; Tunnessen WW Jr
PT - JOURNAL ARTICLE; REVIEW (15 references); REVIEW OF REPORTED CASES
AB - BACKGROUND--Discoid lupus erythematosus (DLE) is uncommon in
childhood. Less than 2% of patients with DLE develop the disease before 10
years of age. OBSERVATIONS--We present eight cases of childhood DLE with
onset before age 10 years: four black boys with cutaneous DLE, three black
girls ages 7, 2, and 6 years at onset, who developed systemic lupus
erythematosus at ages 12, 9, and 8 years, respectively, and a 10-year-old
Hispanic boy who had a systemic flare at the age of 20 years.
CONCLUSIONS--A review of the 16 published cases of childhood DLE reveals
that it is similar to its adult counterpart in its presentation and chronic
course. However, several important differences are noted: a lack of female
predominance, a low incidence of photosensitivity, and frequent progression
to systemic lupus erythematosus at an early age. A discussion of the
management of DLE in children is also presented.
=====================================================================
33.) Warts and lupus erythematosus.
=====================================================================
SO - Lupus 1993 Feb;2(1):21-3
AU - Yell JA; Burge SM
PT - JOURNAL ARTICLE
AB - The human papilloma virus is implicated in causing several diseases,
ranging from the common wart to malignancy. We describe a high prevalence
of cutaneous warts in lupus erythematosus. The presence of warts did not
correlate with the taking of immunosuppressive drugs. This observation
suggests that there is a primary immunological defect among patients with
lupus erythematosus. We found this high rate among patients with discoid as
well as systemic lupus erythematosus. We found no correlation between the
prevalence of cutaneous warts and cervical dysplasia, or malignancy.
Discoid lupus erythematosus is often considered to be a different disease
from systemic lupus erythematosus, running a more benign course. The high
prevalence of cutaneous warts in both conditions highlights yet another
similarity between these two diseases.
=====================================================================
34.) Systemic sclerosis (scleroderma) associated with discoid lupus
erythematosus.
=====================================================================
SO - Dermatology 1993;187(3):178-81
AU - Sasaki T; Nakajima H
PT - JOURNAL ARTICLE
AB - Six patients with systemic sclerosis (SS) and discoid lupus
erythematosus (DLE) were studied to determine whether such cases have some
common clinical and laboratory findings. DLE preceded SS in all cases.
Three patients had diffuse scleroderma with lung and esophagus involvements
and the others limited scleroderma. Three patients had anti-topoisomerase-I
and antiribonucleoprotein antibodies, 2 had either of them and the
remaining anticentromere antibodies. Four had DLE located on the scalp,
leading to alopecia. The other 2 had DLE on the face and extremities. No
case fulfilled criteria for systemic lupus erythematosus (SLE). The present
cases with SS and DLE, but without SLE, indicate that this type of
systemic-cutaneous collagen disease overlap does exist and may be not so rare.
=====================================================================
35.) Vitamin E and discoid lupus erythematosus.
=====================================================================
SO - Lupus 1992 Oct;1(5):303-5
AU - Yell JA; Burge S; Wojnarowska F
PT - CLINICAL TRIAL; JOURNAL ARTICLE
AB - We treated seven patients with discoid lupus erythematosus (DLE) with
Vitamin E in an oral dose of 400 mg three times per day for 12 weeks. All
other systemic and topical treatments were discontinued 1 month before
initiation of the trial. The drug was then stopped and follow-up continued
for at least another 4 weeks. No patient showed clearing of lesions. The
trial was conducted during summer, when DLE is likely to be most active.
There was no deterioration in any patient. No side effects were noted.
=====================================================================
36.) Clinical, histologic, and immunofluorescent distinctions between
subacute cutaneous lupus erythematosus and discoid lupus erythematosus.
=====================================================================
SO - J Invest Dermatol 1992 Sep;99(3):251-7
AU - David-Bajar KM; Bennion SD; De Spain JD; Golitz LE; Lee LA
PT - JOURNAL ARTICLE
AB - Subacute cutaneous lupus erythematosus (SCLE) was originally
described and distinguished from discoid lupus erythematosus (DLE) on the
basis of clinical examination of the skin, but subsequent reports have
questioned the concept of SCLE as a marker of a unique subset of LE
patients. We classified 27 lupus patients, on the basis of cutaneous exam,
as having discoid lupus skin lesions, subacute cutaneous skin lesions, or
systemic lupus erythematosus (SLE) without DLE or SCLE lesions. Clinical
features most characteristic of SCLE rather than DLE were superficial,
non-indurated, non-scarring lesions, and photosensitivity, with lack of
induration being the single most helpful finding. Histologic examination of
lesional skin showed a relatively sparse, superficial infiltrate in SCLE
and a denser, deeper infiltrate in DLE. A distinctive pattern of staining
with direct immunofluorescence, particulate epidermal IgG deposition, was
found in seven of seven SCLE patients (all anti-Ro/SSA positive) and none
of the other patients. This distinctive pattern can be reproduced
experimentally when anti-Ro/SSA autoantibodies are infused into human
skin-grafted mice. Particulate dermal-epidermal junctional staining was the
pattern seen in the patients who did not have SCLE. Clinically defining
SCLE as a superficial inflammatory form of cutaneous lupus (i.e.,
considering lesions to be DLE if they are indurated) results in a
meaningful segregation of SCLE and DLE patient groups. The epidermal IgG
deposits unique to SCLE provide independent evidence that the clinical
findings that were used to identify the patient groups actually identify
distinctive cutaneous lupus subsets. The observation that antibodies are
present in a different location in the skin in SCLE than in DLE indicates
that SCLE and DLE are likely to have different pathomechanisms.
=====================================================================
37.) Scarring alopecia in discoid lupus erythematosus.
=====================================================================
SO - Br J Dermatol 1992 Apr;126(4):307-14
AU - Wilson CL; Burge SM; Dean D; Dawber RP
PT - JOURNAL ARTICLE
AB - The clinicopathological features of the scarring alopecia of discoid
lupus erythematosus (DLE) were studied. Scarring alopecia was present in
34% of 89 patients with DLE and was associated with a prolonged disease
course. More than half these patients had scalp involvement at the onset of
the disease. There was a significant reduction in size of sebaceous glands
in affected scalp. Perifollicular lymphocytic inflammation was maximal
around the mid-follicle at the level of the sebaceous gland, which seems to
be an important functional level in the follicle. There are changes in the
expression of the matrix molecules, the proteoglycans, in the connective
tissue sheath and the keratin intermediate filaments in the outer root
sheath cells at this level in normal scalp and in diseased scalp. Loss of a
population of mid-follicular stem cells may be important in the
pathogenesis of scarring alopecia in DLE.
=====================================================================
38.) Cutaneous lupus erythematosus in India: immunofluorescence profile
[see comments]
=====================================================================
CM - Comment in: Int J Dermatol 1993 Jan; 32(1):76
SO - Int J Dermatol 1992 Apr;31(4):265-9
AU - George R; Mathai R; Kurian S
PT - JOURNAL ARTICLE
AB - The clinical profile and cutaneous lesions of 65 patients with lupus
erythematosus (LE) are described. This included 28 discoid LE (13
disseminated, 15 localized), five subacute cutaneous LE, and 32 systemic
LE. The need to recognize a pigmented macular form constituting 25% of
discoid LE is emphasized. Increased incidence of involvement of the lower
lip in discoid LE and pigmentation in systemic LE is noted. Lupus band test
was found to be highly sensitive; it was positive for lesional skin of all
untreated patients with subacute cutaneous LE and systemic LE, it was,
however, not useful on nonlesional skin.
=====================================================================
39.) Chilblain lupus erythematosus: report of 15 cases [see comments]
=====================================================================
CM - Comment in: Dermatology 1992; 185(2):160
SO - Dermatology 1992;184(1):26-8
AU - Doutre MS; Beylot C; Beylot J; Pompougnac E; Royer P
PT - JOURNAL ARTICLE
AB - In this retrospective study, the authors describe the clinical,
histologic and laboratory features of 15 cases of chilblain or perniotic
lupus. In winter, the patients (14 women, 1 man) develop chilblain-like
lesions, chiefly in the toes (8 times) and fingers (11 times). Histologic
features are identical to those of discoid lupus erythematosus. The damaged
skin gives a positive fluorescent band test. Usually, these lesions occur
in association with discoid lupus of the face. However, in 8 patients, they
were the only cutaneous sign of lupus. This form of lupus can evolve to a
systemic form, as was the case with 3 patients.
=====================================================================
40.) Sweat gland abnormalities in lichenoid dermatosis.
=====================================================================
SO - Histopathology 1991 Oct;19(4):345-9
AU - Akosa AB; Lampert IA
PT - JOURNAL ARTICLE
AB - Lichenoid dermatosis is a pattern description of a variety of
cutaneous lesions which primarily affect the dermoepidermal junction.
Involvement of skin appendages has been restricted to hair follicles in
lichen planopilaris and discoid lupus erythematosus. Sweat gland
involvement has not been described in the four common members of this
group, namely, lichen planus, discoid lupus erythematosus, fixed drug
eruptions and erythema multiforme, although structural abnormalities have
been reported in graft-versus-host disease. In a detailed morphological
study of 59 cases, including lichen planus (12), discoid lupus
erythematosus (18), fixed drug eruption (14) and erythema multiforme (15),
78% (47/59) showed sweat, gland abnormalities. The abnormalities included
vacuolation of cell cytoplasm, with and without lymphocytic infiltration,
apoptosis of basal cells and basal cell hyperplasia of the excretory ducts
which predominantly affected the portion of the duct adjoining the
acrosyringium. The portion of the duct close to the secretory gland was
only involved in continuity and the secretory glands were unaffected. These
abnormalities of the sweat gland mostly constitute primary involvement by
the disease process in contrast to structural abnormalities secondary to
fibrosis.
=====================================================================
41.) The progressive systemic sclerosis/systemic lupus overlap: an unusual
clinical progression.
=====================================================================
SO - Ann Rheum Dis 1991 May;50(5):323-7
AU - Asherson RA; Angus H; Mathews JA; Meyers O; Hughes GR
PT - JOURNAL ARTICLE
AB - Three patients with the unusual combinations of discoid lupus,
systemic lupus erythematosus (SLE), and progressive systemic sclerosis
(PSS) are reported. The first patient developed PSS eight years after a
diagnosis of discoid lupus had been made and this was complicated by
myositis six years later. The second patient developed PSS more than 20
years after being diagnosed as having SLE. The third patient developed SLE
with predominant features of urticarial vasculitis six years after PSS.
Mild myositis also ensued. There were no antibodies to U1RNP demonstrable
in any of these patients. The clinical progression of SLE to PSS or vice
versa in the absence of features of mixed connective tissue disease is
distinctly uncommon.
=====================================================================
42.) Safety and efficacy of a broad-spectrum sunscreen in patients with
discoid or subacute cutaneous lupus erythematosus.
=====================================================================
SO - Cutis 1991 Feb;47(2):130-2, 135-6
AU - Callen JP; Roth DE; McGrath C; Dromgoole SH
PT - JOURNAL ARTICLE
AB - An eight-week, open-label study was conducted to test the efficacy,
safety, and cosmetic acceptability of a broad-spectrum sunscreen in
patients with discoid lupus erythematosus or subacute cutaneous lupus
erythematosus. The sunscreen combined the ultraviolet A absorber avobenzone
(Parsol 1789, Givaudan Corp) and the ultraviolet B absorber padimate O and
had a sun protection factor greater than fifteen. The overall clinical
disease severity decreased from 2.7 (four point scale) at baseline to 1.7
after eight weeks (p = 0.005). Cutaneous signs and symptoms, including
hyperpigmentation, papules, scaling, and erythema, were significantly less
severe at the end of the study. The level of protection provided by the
sunscreen was good to excellent in 54 percent of patients, and was judged
to be superior or far superior to previously used sun protection
factor-fifteen sunscreens in 77 percent of patients. Most patients found
the sunscreen highly acceptable with respect to its cosmetic properties.
=====================================================================
43.) Hereditary deficiency of C5 in association with discoid lupus
erythematosus.
=====================================================================
SO - J Am Acad Dermatol 1991 Feb;24(2 Pt 2):376-8
AU - Asghar SS; Venneker GT; van Meegen M; Meinardi MM; Hulsmans RF; de
Waal LP
PT - JOURNAL ARTICLE
AB - A 29-year-old woman with discoid lupus erythematosus had undetectable
classic pathway complement activity. Hypocomplementemia was due to
selective deficiency of C5. One of her children was also deficient. To our
knowledge this is the first documented case of an association between
discoid lupus erythematosus and C5 deficiency.
=====================================================================
44.) Response of discoid and subacute cutaneous lupus erythematosus to
recombinant interferon alpha 2a.
=====================================================================
SO - J Invest Dermatol 1990 Dec;95(6 Suppl):142S-145S
AU - Nicolas JF; Thivolet J; Kanitakis J; Lyonnet S
PT - JOURNAL ARTICLE
AB - Ten patients suffering from discoid lupus erythematosus (DLE) or
subacute cutaneous lupus erythematosus (SCLE) were treated with interferon
alpha 2a. A marked improvement or clearing of cutaneous lupus erythematosus
lesions was observed in eight of them. However, the response to interferon
was of short duration and within a few weeks after interferon withdrawal
all patients who were improved or cleared relapsed. This study suggests
that interferon alpha 2a represents a new interesting approach in the
treatment of DLE and SCLE. Ongoing trials will define the optimal treatment
schedule for the maintenance of interferon-induced improvement of cutaneous
lupus erythematosus.
=====================================================================
45.) Recombinant interferon alpha 2a is effective in the treatment of
discoid and subacute cutaneous lupus erythematosus.
=====================================================================
SO - Br J Dermatol 1990 Mar;122(3):405-9
AU - Thivolet J; Nicolas JF; Kanitakis J; Lyonnet S; Chouvet B
PT - CLINICAL TRIAL; JOURNAL ARTICLE
AB - Ten patients suffering from either discoid lupus erythematosus (DLE)
or subacute cutaneous lupus erythematosus (SCLE) were treated with
interferon alpha 2a. Eight received low or intermediate doses (18-45 x
10(6) U/week) for a short period of time (4-8 weeks), with marked
improvement of skin lesions in six, an exacerbation in one patient and no
change in the other. Two patients with SCLE received high doses (100-120 x
10(6) U/week) over 12 weeks, with complete clearing of the lesions in one
and a marked improvement in the other. The responses were of short duration
and within a few weeks of stopping treatment all who had improved or
cleared relapsed. The side-effects in all the patients were fever and a
flu-like syndrome which necessitated a reduction of the dose in one case.
In two patients there were increases in the liver enzyme levels, but no
haematological toxicity was noted.
=====================================================================
46.) Experimental reproduction of skin lesions in lupus erythematosus by
UVA and UVB radiation [see comments]
=====================================================================
CM - Comment in: J Am Acad Dermatol 1991 Mar; 24(3):515
SO - J Am Acad Dermatol 1990 Feb;22(2 Pt 1):181-7
AU - Lehmann P; Holzle E; Kind P; Goerz G; Plewig G
PT - JOURNAL ARTICLE
AB - Sunlight is a well-established factor in the induction and
exacerbation of lupus erythematosus. Although experimental reproduction of
lupus erythematosus lesions with wavelengths shorter than 320 nm was
demonstrated previously, the effect of wavelengths longer than 320 nm was
not investigated adequately. In this study we show that the action spectrum
of lupus erythematosus reaches into the UVA region. A total of 128 patients
with lupus erythematosus underwent phototesting with the use of
polychromatic UVB and long-wave UVA. Subsets of the disease consisted of
discoid lupus erythematosus (n = 86), subacute cutaneous lupus
erythematosus (n = 22), and systemic lupus erythematosus (n = 20). Skin
lesions clinically and histologically compatible with lupus erythematosus
were induced in 64% of patients with subacute cutaneous lupus
erythematosus, 42% of patients with discoid lupus erythematosus, and 25% of
patients with systemic lupus erythematosus. The action spectrum of the
induced lesions was within the UVB range in 33% of patients, in the UVA
range in 14%, and in the UVB and UVA range in 53%. In positive test
reactions patchy dark erythema and urticarial plaques developed within a
few days. In some patients typical discoid lesions persisted for months.
=====================================================================
47.) Histopathologic comparison of the subsets of lupus erythematosus [see
comments]
=====================================================================
CM - Comment in: Arch Dermatol 1990 Dec; 126(12):1651
SO - Arch Dermatol 1990 Jan;126(1):52-5
AU - Jerdan MS; Hood AF; Moore GW; Callen JP
PT - JOURNAL ARTICLE
AB - A recent study by Bangert et al suggests that there are quantitative
histologic differences that distinguish discoid lupus erythematosus (DLE)
and subacute cutaneous lupus erythematosus (SCLE). Utilizing criteria
proposed by these authors, we examined 77 biopsy specimens from 63 patients
with various forms of lupus erythematosus, but we were unable to predict
the correct clinical subset. Using the clinical diagnosis of DLE as a
positive reference standard, the sensitivity and specificity for the
overall pathologic diagnosis of DLE were 55% and 42%, respectively.
Statistically significant histologic factors favoring the diagnosis of DLE
over SCLE in the present study were pilosebaceous atrophy, hyperkeratosis,
parakeratosis, basement membrane thickening around the follicles,
subepidermal edema, and vascular ectasia. These histologic variables were
entered into a forward stepwise multivariate regression analysis to
determine distinct predictors of DLE vs SCLE. This analysis showed that
pilosebaceous atrophy was the only distinct significant predictor of DLE vs
SCLE. These results suggest that the histologic differentiation of
clinically defined DLE and SCLE cannot be established from the histologic
features examined.
=====================================================================
48.) Chronic cutaneous lupus erythematosus.
=====================================================================
SO - Med Clin North Am 1989 Sep;73(5):1055-71
AU - Hymes SR; Jordon RE
PT - JOURNAL ARTICLE; REVIEW (60 references); REVIEW, TUTORIAL
AB - Chronic cutaneous LE is a diverse disease, characterized by
predominantly cutaneous disease with few systemic complications. Discoid
lesions are commonly seen, but they are not specific for chronic cutaneous
LE. These scarring and disfiguring changes are also present in neonatal LE,
SLE, and complement deficiency LE. Because definitive diagnosis cannot be
made by cutaneous examination alone, all patients should initially be
evaluated for systemic disease. A small percentage of patients with chronic
cutaneous LE will ultimately develop SLE, and therefore, patients should be
re-evaluated periodically. The pathogenesis of the cutaneous lesions is not
definitively known. There is suggestive evidence implicating T-cell
mediated injury, especially in discoid LE. Antibody-dependent cellular
cytotoxicity may also play a significant role in cellular damage in
subacute cutaneous LE and neonatal LE, especially in the presence of
anti-Ro antibody. Immunoglobulin deposition in association with membrane
attack complex, has been associated with epidermal injury in some cases.
Treatment of chronic cutaneous LE is largely symptomatic and nonspecific,
focusing on reduction of inflammation. Further knowledge of pathogenesis
will, hopefully, provide for specific immunologic therapy.
=====================================================================
49.) Rowell's syndrome. Report of a case.
=====================================================================
SO - J Am Acad Dermatol 1989 Aug;21(2 Pt 2):374-7
AU - Parodi A; Drago EF; Varaldo G; Rebora A
PT - JOURNAL ARTICLE; REVIEW (8 references); REVIEW, TUTORIAL
AB - We describe a patient with discoid lupus erythematosus who developed
annular lesions of the thigh and chilblainlike lesions of the fingers
matching those described in the original reports of Rowell's syndrome. The
patient also had circulating anti-Ro(SS-A) antibodies whose similarity to
the anti-Sj-T antibodies found in the original Rowell's syndrome cases has
been recently claimed. A review of the literature suggests that most of the
cases of Rowell's syndrome described thus far in fact may be cases of
coincidental association of lupus erythematosus and erythema multiforme.
=====================================================================
50.) Expression of lymphocyte activation markers in benign cutaneous T cell
infiltrates. Discoid lupus erythematosus versus lichen ruber planus.
=====================================================================
SO - Acta Derm Venereol 1989;69(4):292-5
AU - Sundqvist KG; Wanger L
PT - JOURNAL ARTICLE
AB - The expression of lymphocyte activation markers (IL2 receptors,
transferrin receptors and HLA-DR) was examined in cutaneous lymphoid
infiltrates of 12 patients with lichen ruber planus (LP) and 10 individuals
with discoid lupus erythematosus (DLE). The cell infiltrates in both
conditions were generally of considerable size. The vast majority of the
infiltrating cells were T cells. The reactivity of the anti-IL2 receptor
antibody used was confined to lymphocytes. In patients with LP 26 +/- 17%
of the infiltrating cells were IL2 receptor positive, 20 +/- 8% carried
transferrin receptors and greater than 90% HLA-DR. In patients with DLE
less than 1% were IL2 receptor positive, less than 5% carried transferrin
receptors and greater than 90% were HLA-DR positive. These data indicate
that IL2 receptor expression distinguishes the infiltrating T-lymphocytes
in LP and DLE, although in both conditions the vast majority of the
infiltrating cells were activated as revealed by their expression of HLA-DR.
=====================================================================
51.) [Congenital ischemic onychodystrophy (Iso-Kikuchi syndrome) and
chronic lupus
=====================================================================
erythematosus]
SO - Hautarzt 1988 Nov;39(11):750-2
AU - Bittar EQ; Parra CA; Ledesma de Prieto G; Briggs E; Ortiz Baeza O
PT - JOURNAL ARTICLE
AB - We report a patient with nail and bone disorders of the index and
middle fingers (Iso and Kikuchi syndrome) associated with chronic discoid
lupus erythematosus. Angiographic studies showed filiform arteries of the
fingers and slow blood circulation. Since a vascular pathogenic mechanisms
is probable, the designation "Congenital ischemic onychodystrophy" seems
more suitable. The association with chronic discoid lupus erythematosus has
not previously been reported.
=====================================================================
52.) Evaluation of lymphocyte activation in skin lesions of patients with
mixed connective tissue disease and discoid lupus erythematodes.
=====================================================================
SO - Arch Dermatol Res 1988;280(1):1-4
AU - Bergroth V; Konttinen YT; Piirainen H; Johansson E; Nordstrom D;
Malmstrom M
PT - JOURNAL ARTICLE
AB - Biopsy specimens from mixed connective tissue disease (MCTD) and
discoid lupus erythematodes (DLE) skin lesions were stained with monoclonal
antibodies to differentiation and activation antigens. In addition, the
blast cells were studied by combining autoradiography with immunoperoxidase
staining. In both disease conditions most of the inflammatory cells in situ
were positive for T11 antigen, the CD4/CD8 ratio being low. Only a few of
the cells were pan-B positive B cells. The expression of various activation
antigens did not differ significantly between MCTD and DLE biopsy
specimens; the number of T9, Tac, and 4F2 antigen carrying cells was
relatively low, whereas Ia-positive cells were more numerous. 3H-Thymidine
incorporating T blasts comprised less than 1% of all inflammatory cells. T4
and T8 marker-carrying blast cells were present in about equal proportions.
These findings suggest that Ia antigen-expressing T cells are important
from the pathogenetic point of view in both MCTD and DLE. Because the local
proliferation of T cells was extremely low according to the lack of
interleukin-2 receptor and OKT9 markers and 3H-thymidine incorporation, it
seems probable that most of the T cells are recruited from the circulation
to the site of the inflammation.
=====================================================================
53.) Autofluorescence of clofazimine in discoid lupus erythematosus.
=====================================================================
SO - J Am Acad Dermatol 1987 Nov;17(5 Pt 2):867-71
AU - Kossard S; Doherty E; McColl I; Ryman W
PT - JOURNAL ARTICLE
AB - A 70-year-old woman developed dark reddish blue pigmentation in
scarred areas of discoid lupus erythematosus after taking clofazimine
intermittently over a period of 10 years. Although light microscopy of
routinely processed tissue failed to define the cause of the pigment,
fluorescent microscopy showed vivid red deposits concentrated around larger
vessels within the dermis. These deposits were shown to correspond to
birefringent red clofazimine crystals on fresh frozen sections. Although
the hyperpigmentation may clinically resemble melanin, biopsy specimens
from our patient revealed a loss of melanin pigment in lesional skin,
suggesting a primary role for clofazimine in producing the color changes
observed.
=====================================================================
54.) A family survey of lupus erythematosus. 1. Heritability.
=====================================================================
SO - J Rheumatol 1987 Oct;14(5):913-21
AU - Lawrence JS; Martins CL; Drake GL
PT - JOURNAL ARTICLE
AB - First degree relatives and spouses of 36 patients with systemic lupus
erythematosus (SLE) and 37 with discoid lupus erythematosus (LE) were
assessed using the ARA criteria. They were compared with relatives and
spouses of patients with other rheumatic and related complaints. Definite
SLE was present in 3.9% of relatives of SLE probands, 2.6% of discoid
relatives and 0.3% of controls. Discoid LE was diagnosed in 0.6% of SLE and
3.5% of discoid families compared with 0.5% of controls. None of the
spouses of LE probands had SLE or discoid LE. The data gave the best fit
for a polygenic inheritance with a heritability of 66 +/- 11% for SLE and
44 +/- 10% for discoid LE. Genetic factors are thus less important in SLE
and discoid LE than in generalized osteoarthritis, spondylitis or gout with
heritabilities of 90, 72 and 90%, respectively.
=====================================================================
56.) A comparison of the dermal lymphoid infiltrates in discoid lupus
erythematosus and Jessner's lymphocytic infiltrate of the skin using the
monoclonal antibody Leu 8.
=====================================================================
SO - J Cutan Pathol 1987 Aug;14(4):198-201
AU - Ashworth J; Turbitt M; MacKie R
PT - JOURNAL ARTICLE
AB - Jessners lymphocytic infiltration of the skin (14 cases) and discoid
lupus erythematosus (13 cases) were studied and the lymphoid infiltrates in
the dermis were compared in the two conditions, using a standard
immunoperoxidase technique. Mouse monoclonal antibodies were used to
identify T helper lymphocytes, T suppressor lymphocytes and, using the
antibody Leu 8, "immunoregulatory lymphocytes". It was shown that the
proportions of Leu 8 positive cells was significantly different in the two
conditions. The average percentage of Leu 8 positive lymphocytes in the
dermal infiltrate found in the cases of Jessner's was 65% (range 40-80%)
whereas the average percentage in the cases of discoid LE was 15% (range
2-30%). This observation is further evidence that Jessner's lymphocytic
infiltration and chronic discoid lupus erythematosus should be regarded as
separate entities.
=====================================================================
57.) Lupus profundus in children: treatment with hydroxychloroquine.
=====================================================================
SO - J Am Acad Dermatol 1987 Apr;16(4):839-44
AU - Fox JN; Klapman MH; Rowe L
PT - JOURNAL ARTICLE
AB - Discoid lupus erythematosus and lupus profundus, rare in children,
are described in two young girls, one with onset at 3 1/2 years of age, the
other at 8 years of age. Unusual nodules of the face that ultimately healed
with atrophy and hyperpigmentation showed histologic and immunofluorescent
confirmation of lupus erythematosus. These patients, the second and third
in the English literature to be treated for childhood lupus profundus with
antimalarials, responded successfully to hydroxychloroquine. No systemic
involvement was found.
=====================================================================
58.) The reliability of immunofluorescence and histopathology in the
diagnosis of discoid lupus erythematosus and lichen planus.
=====================================================================
SO - Br J Dermatol 1987 Feb;116(2):189-98
AU - Nieboer C
PT - JOURNAL ARTICLE
AB - We have investigated the diagnostic reliability of the
immunofluorescence (IF) technique and histopathology in discoid lupus
erythematosus (DLE) and lichen planus (LP) and in diseases clinically
resembling these (DLE-like and LP-like). In all cases of DLE and LP it was
possible to establish the clinical diagnosis with one or both methods, when
in initially negative cases the investigations were repeated on fresh
biopsies. In DLE the diagnostic specificity of IF was greater than that of
histopathology, and the diagnostic sensitivity of the results of both
methods together was greater than that of the two methods separately. In LP
the diagnostic specificity of both methods was maximal, but IF showed
greater diagnostic sensitivity. These differences were not statistically
significant. The most important immunohistochemical feature for diagnosis
by IF was the incidence and the morphological pattern of IgG along the
epidermal basement membrane. This held true for differentiation between LP
and DLE and also between DLE and DLE-like diseases. Combination of the
results of IF and histopathology gave the most reliable results in DLE. In
LP, IF was more reliable than histopathology.
=====================================================================
59.) Immunopathology of cutaneous human lupus erythematosus defined by
murine monoclonal antibodies.
=====================================================================
SO - J Am Acad Dermatol 1986 Sep;15(3):474-81
AU - Andrews BS; Schenk A; Barr R; Friou G; Mirick G; Ross P
PT - JOURNAL ARTICLE
AB - Skin biopsy specimens obtained from involved skin from sixteen
patients with systemic and discoid lupus erythematosus were studied. Murine
monoclonal antibodies with a biotin-avidin-horseradish peroxidase staining
system were used. The findings consisted of a marked reduction in the
number of epidermal Langerhans cells defined by surface antigens, reduced
HLA-DR (Ia-like) antigens on the surface of dermal capillary endothelium,
and mononuclear cell infiltrates characterized by a predominance of helper
T lymphocytes and an increase in the number of mononuclear phagocytic
cells. B lymphocytes were rarely identified. The number of T lymphocytes
within the dermis correlated inversely with both the number of
HLA-DR-positive epidermal Langerhans cells (p less than 0.01) and the
HLA-DR staining of dermal capillary endothelium (p less than 0.01). These
findings suggest that a T lymphocyte-mediated immune response associated
with a reduction in Langerhans cells and capillary endothelium HLA-DR
antigens is involved in the inflammatory process of lupus erythematosus skin.
=====================================================================
60.) HLA genotypes in a family with a case of homozygous C2 deficiency and
discoid lupus erythematosus.
=====================================================================
SO - Acta Derm Venereol 1986;66(5):419-22
AU - Braathen LR; Bratlie A; Teisberg P
PT - JOURNAL ARTICLE
AB - A fifty-year-old man with a history of recurrent bronchial and renal
infections, and rheumatoid arthritis was admitted with a
sunexposure-induced discoid lupus erythematosus. Complement levels and HLA
typing of the patient and his family revealed a homozygous C2 deficiency in
the patient and his HLA-identical healthy younger sister. The C2 deficiency
gene was associated with HLA-A10, B18, DR2, C4A4B2, BfS on one chromosome
and with HLA-A2, B7, DR2, C4A4B2, BfS on the other.
=====================================================================
61.) Laser treatment of discoid lupus (case report).
=====================================================================
SO - Lasers Surg Med 1986;6(1):12-5, 44-5
AU - Henderson DL; Odom JC
PT - JOURNAL ARTICLE
AB - This is a case report of vaporization of the characteristic
disfiguring plaques of discoid lupus erythematosus (DLE) with the carbon
dioxide laser. This patient had a dramatic clinical and cosmetic
improvement. It is suggested that the altered but not vaporized cells that
remained were responsible for the retardation of the disease process.
=====================================================================
62.) Serologic and clinical features of patients with discoid lupus
erythematosus: relationship of antibodies to single-stranded
deoxyribonucleic acid and of other antinuclear antibody subsets to clinical
manifestations.
=====================================================================
SO - J Am Acad Dermatol 1985 Nov;13(5 Pt 1):748-55
AU - Callen JP; Fowler JF; Kulick KB
PT - JOURNAL ARTICLE
AB - Serologic and clinical data were obtained from forty patients with
discoid lupus erythematosus in 1982. Clinical disease was characterized by
quality, extent, severity, activity, photosensitivity, and systemic
manifestations. The patient's sera were examined for the presence of
antinuclear, anti-Ro and anti-La, anti-ribonucleoprotein and anti-Sm,
anti-single-stranded deoxyribonucleic acid (ssDNA), and antinative DNA
antibodies. In late 1984, thirty-three patients had follow-up clinical
examinations. On the initial evaluation the patients with positive
antinuclear antibody (ANA) findings were clinically characterized by a
significantly higher incidence of photosensitivity and arthritis, an
elevated erythrocyte sedimentation rate, and cutaneous lesions of subacute
cutaneous lupus erythematosus. The activity and extent of disease in 1982
did not correlate with the presence of ANA. Elevated levels of ssDNA
antibodies were present in seven of the forty patients (significantly
greater than control subjects; (p less than 0.005) and correlated with
widespread, active discoid lupus erythematosus, an elevated erythrocyte
sedimentation rate, and a slightly greater risk of systemic lupus
erythematosus in 1982. At the 2-year follow-up examination, thirteen of the
seventeen patients with a positive ANA had active clinical cutaneous
disease, and ten of the sixteen patients with negative ANA findings had
continued activity (not statistically significant). However, all seven
patients with elevated ssDNA antibody levels had continued activity, and
disease progression had occurred in three. Thus the presence of ssDNA seems
to correlate strongly with active, progressive lupus erythematosus. The
presence of antibody abnormalities in patients with discoid lupus
erythematosus correlates with clinical disease and provides more support
for the theory linking discoid lupus erythematosus to systemic lupus
erythematosus as part of a continuum.
=====================================================================
63.) Squamous cell carcinoma of the lip developing in discoid lupus
erythematosus.
=====================================================================
SO - Oral Surg Oral Med Oral Pathol 1985 Oct;60(4):382-6
AU - Handlers JP; Abrams AM; Aberle AM; Auyong T; Melrose RJ
PT - JOURNAL ARTICLE
AB - Since the substitution of steroids and antimalarials for irradiation
in the treatment of discoid lupus erythematosus, squamous cell carcinoma
arising in discoid lupus erythematosus is thought by some to be an uncommon
occurrence. A review of the recent literature (subsequent to 1945) revealed
fifteen cases, of which seven occurred in the lips. In one of twelve of the
cases a history of irradiation was documented. In three other cases, there
was no evidence of its use. We report an additional case of squamous cell
carcinoma occurring in the lower lip of a 24-year-old black woman in the
absence of radiation therapy. A review of the literature and a discussion
of possible predisposing factors are presented.
======================================================================
DATA-MEDICOS/DERMAGIC-EXPRESS No (52) 05/05/99 DR. JOSE LAPENTA R.
======================================================================
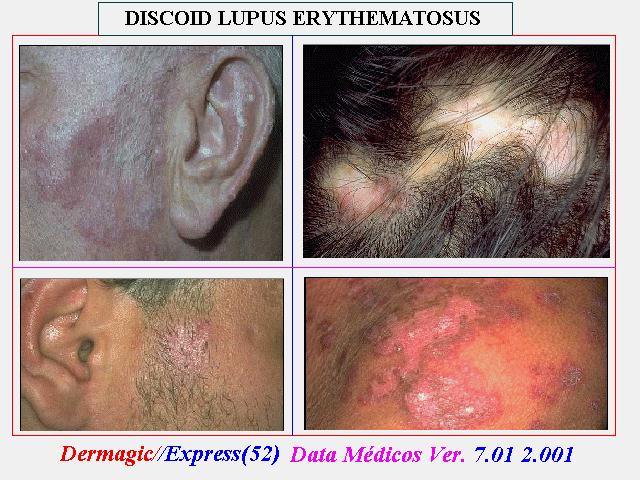
|