| The melasma II,
it really disapears definively or it is a fantasy ?.
El Melasma II, realmente
curable, o es una fantasia ?
Data-Medicos
Dermagic/Express No. 3-(97)
27 Febrero 2.001.27 February 2.001.
EDITORIAL ESPANOL
=================
Hola a todos los amigos DERMATOLOGOS de mundo !!!. El tema de hoy, bastante caliente:
EL MELASMA, REALMENTE DESAPARECE DEFINITIVAMENTE O ES UNA FANTASIA ?
Cuenta la historia que el primer BLANQUEADOR PARA LA PIEL fue descubierto casualmente por PILOTOS DE AVIONES DE COMBATE, en cuyas mascarillas de goma iba incluido UN COMPONENTE que blanqueba la PIEL, se estudio el componente y se aislo, asi nacio la hidroquinona como blanqueador. Luego de ella han venido otros mas, como el acido retinoico, de COMPROBADA EFECTIVIDAD, los esteroides topicos, el acido glicolico, fitico, kojico, peelings, ultimamente el laser, y otros mas.
Para todo dermatologo es un reto jugar con estos componentes para lograr el aclaramiento de las manchas sobre todo en las mujeres, quienes quieren siempre tener un rostro bello. En buena medida figuran importantemente el USO DE BUENOS PROTECTORES SOLARES, no exponerse a la luz solar excesivamente, no usar mucho maquillaje, y por supuesto las FORMULACIONES MAGISTRALES que cada quien tiene en su armamento DERMATOLOGICO.
Ultimamente se ha tratado de relacionar el melasma con el HELYCOBACTER PYLORI. Pero les cuento que en mi viaje por la internet NO ENCONTRE NINGUN TRABAJO CIENTIFICO ALUSIVO A ESTE TEMA. Yo humildemente DUDO 100% que el MELASMA tenga algo que ver CON dicho AGENTE VIVO. Pienso que el melasma en buena medida se debe a cuatro factores importantes:
1.) SENSIBILIDAD CUTANEA A LA LUZ SOLAR.
2.) USO DE MAQUILLAJE Y PERFUME EN LA CARA SIN PROTECTORES SOLARES
3.) EXPOSICION PROLONGADA AL SOL.
4.) PREDISPOSICION GENETICAMENTE DETERMINADA.
El objetivo de esta revision, ademas de revisar que hay de nuevo y que elementos se estan usando ACTUALMENTE EN EL MELASMA. Era responder esa pregunta que les hago hoy a TODOS:
REALMENTE HAY ALGUN TRATAMIENTO QUE LO ELIMINE 100% Y NO VUELVA A APARECER, ??? Pues segun todas estas referencias bibliograficas, EL MELASMA MEJORA con el uso racional de todos estos elementos. PERO QUE PASA SI EL PACIENTE ABANDONA EL PROTECOR SOLAR, o DEJA DE COLOCARSE su crema de ACIDO RETINOICO O GLICOLICO EN LAS NOCHES ,,,, y se VA PARA LA PLAYA a darse un buen bronceado ???... ustedes lo saben mejor que yo. EL MELASMA VUELVE A APARECER.
Por alli he leido EN REVISTAS TRATAMIENTOS Y CREMAS MAGICAS que hacen desaparecer el MELASMA, a COSTOS ELEVADISIMOS, cremas con nombres HERMOSOS, tratamientos GARANTIZADOS,,,, Por supuesto MIENTRAS NO DEJEN DE USAR LA CREMITA CON BLANQUEADOR EN LA NOCHE Y EL PROTECTOR SOLAR EN EL DIA,,,, TODO MELASMA ES "CURABLE"....
Por cierto hoy vi una paciente en la consulta con melasma, tenia tratamientos previos con: hidroquinona, acido retinoico, peelings con acido glicolico, y laser,,,, despues de todo esto LAS MANCHAS VOLVIERON al abandonar el protector solar...y las formulas que le mandaban...
Los hechos en las rererencias...
saludos a todos...
Dr. Jose Lapenta R.
EDITORIAL ENGLISH
=================
Hello to all the friends DERMATOLOGIST of the world !!!. Today's topic, quite hot: Does THE MELASMA, REALLY DISAPPEAR DEFINITIVELY OR is A FANTASY?
All the history that the first BLEACH FOR THE SKIN was discovered accidentally by PILOTS OF AIRPLANES OF COMBATS in whose rubber masks went included A COMPONENT that bleach the SKIN, the component was study and isolates, and she was born this way the hydroquinone like bleach. After her they have come other but, as the retinoic Acid, of PROVEN EFFECTIVENESS, the topical steroids, the glycolic Acid, fitic Acid, kojic Acid, peelings, lately the laser, and other but.
For all dermatologist it is a challenge to play with these components to achieve the clearing of the stains mainly in the women who always want to have a beautiful face. In good measure they figure the USE OF GOOD UN SCREENS importantly, to not be exposed excessively to the solar light, to not use a lot of make-up, and of course the MASTERFUL FORMULATIONS that each who you has in your DERMATOLOGIC armament.
Lately it has been to relate the melasma with the HELYCOBACTER PYLORI. But I can tell you that in my trip for the internet didn't FIND ANY ALLUSIVE SCIENTIFIC WORK TO THIS TOPIC. I lowly DOUBT 100% that the MELASMA has something to do WITH this ALIVE AGENT. I think that the melasma in good measure is due to four important factors:
1.) CUTANEOUS SENSIBILITY TO THE SOLAR LIGHT.
2.) USE OF MAKE-UP AND PERFUME IN THE FACE WITHOUT SOLAR PROTECTORS
3.) LINGERING EXHIBITION in the sun.
4.) PREDISPOSITION GENETICALLY DETERMINATED.
The objective of this revision, besides revising what is NEW and which things are using AT THE MOMENT IN THE MELASMA. It was to respond that question that I make today to ALL:
Is there REALLY SOME TREATMENT THAT ELIMINATES IT 100% AND don't APPEAR again??? Because according to all these bibliographical references, THE MELASMA IMPROVES with the rational use of all these elements. BUT WHAT it HAPPENS IF THE PATIENT ABANDONS THE SOLAR PROTECTOR, or does she STOP to BE PLACED her cream of RETINOIC ACID OR GLYCOLIC IN THE NIGHTS, and does she LEAVE FOR THE BEACH to be given a good suntan ???... you know it better than me. THE MELASMA APPEARS again.
Over there I have read IN MAGAZINES about TREATMENTS AND MAGIC CREAMS that make disappear the MELASMA, at HIGH COSTS, creams with BEAUTIFUL names, GUARANTEED treatments,,,, Of course WHILE they don't STOP to USE THE CREAM WITH BLEACH IN THE NIGHT AND THE SOLAR PROTECTOR IN THE DAY, ALL MELASMA is "CURABLE"....
By the way today I saw a patient in the consultation with melasma, she had previous treatments with: hydroquinone, retinoic acid, peelings with glycolic acid, and laser, after all this THE STAINS RETURNED when abandoning the solar protector ...and the bleach creams that sent her...
The facts, in the references...
Greetings to all...
Dr. José Lapenta R.
=============================================================
REFRENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
=============================================================
1.) Melasma.
2.) Mandibular melasma
3.) Melasma in men. A clinical and histologic study.
4.) Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study.
5.) Retrospective study on the clinical presentation and treatment outcome of melasma in a tertiary dermatological referral centre in Singapore.
6.) Usefulness of retinoic acid in the treatment of melasma.
7.) Topical liquiritin improves melasma.
8.) Erbium:YAG laser resurfacing for refractory melasma.
9.) Association of melasma with thyroid autoimmunity and other thyroidal abnormalities and their relationship to the origin of the melasma.
10.) Topical retinoic acid (tretinoin) for melasma in black patients. A vehicle-controlled clinical trial.
11.) Melasma in men: a hormonal profile.
12.) Topical isotretinoin for melasma in Thai patients: a vehicle-controlled clinical trial.
13.) [Use of a cream based on 20% azelaic acid in the treatment of melasma].
14.) The efficacy of a broad-spectrum sunscreen in the treatment of melasma.
15.) Actinic lichen planus mimicking melasma. A clinical and histopathologic study of three cases.
16.) Glycolic acid peels in the treatment of melasma among Asian women.
17.) Endocrinologic profile of patients with idiopathic melasma.
18.) 5-Fluorouracil as an aid in management of acne and melasma.
19.) Topical tretinoin (retinoic acid) improves melasma. A vehicle-controlled, clinical trial.
20.) Topical tretinoin, hydroquinone, and betamethasone valerate in the therapy of melasma.
21.) Melasma of the forearms.
22.) Treatment of melasma using kojic acid in a gel containing hydroquinone and glycolic acid.
23.) [Melasma in pregnancy: reduction of its appearance with the use of a broad-spectrum photoprotective agent].
24.) Melasma. Etiologic and therapeutic considerations.
25.) Double-blind comparison of azelaic acid and hydroquinone in the treatment of melasma.
26.) N-acetyl-4-S-cysteaminylphenol as a new type of depigmenting agent for the melanoderma of patients with melasma.
27.) Treatment of melasma (chloasma) by local application of a steroid cream.
28.) Hormonal milieu in the maintenance of melasma in fertile women.
29.) Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser.
30.) The combination of glycolic acid and hydroquinone or kojic acid for the treatment of melasma and related conditions.
31.) Intermittent therapy for melasma in Asian patients with combined topical agents (retinoic acid, hydroquinone and hydrocortisone): clinical and histological studies.
32.) Melanin hyperpigmentation of skin: melasma, topical treatment with azelaic acid, and other therapies.
33.) The treatment of melasma. 20% azelaic acid versus 4% hydroquinone cream.
34.) Treatment of melasma with Jessner's solution versus glycolic acid: a comparison of clinical efficacy and evaluation of the predictive ability of Wood's light examination.
35.) The effect of topical tretinoin on the photodamaged skin of the Japanese.
36.) Combination treatment of melasma with pulsed CO2 laser followed by Q-switched alexandrite laser: a pilot study.
37.) The use of chemical peelings in the treatment of different cutaneous hyperpigmentations.
38.) Glycolic acid peels for the treatment of wrinkles and
photoaging.
39.) A possible mechanism of action for azelaic acid in the human epidermis.
40.) A new bleaching protocol for hyperpigmented skin lesions with a high concentration of all-trans retinoic acid aqueous gel.
41.) Experience with a strong bleaching treatment for skin hyperpigmentation in Orientals.
42.)Injection of all-trans retinoic acid for treatment of thin wrinkles.
43.) Embryotoxicity and teratogenicity of topical retinoic acid.
44.) The safety and efficacy of salicylic acid chemical peels in darker racial-ethnic groups.
45.) The combination of 2% 4-hydroxyanisole (Mequinol) and 0.01% tretinoin is effective in improving the appearance of solar lentigines and related hyperpigmented lesions in two double-blind multicenter clinical studies.
46.) Combination of 4-hydroxyanisole and all-trans retinoic acid produces synergistic skin depigmentation in swine.
47.) [Confetti depigmentation following application of Leucodinine B on a chloasma].
48.) Ruby laser treatment of melasma and postinflammatory hyperpigmentation.
49.) The bleachings treatments.
=============================================================
1.) Melasma.
=============================================================
Adv Exp Med Biol 1999;455:491-9
Kauh YC, Zachian TF
Department of Dermatology and Cutaneous Biology, Thomas Jefferson University, Jefferson Medical College, Philadelphia, Pennsylvania 19107, USA. [email protected]
Melasma is a common disorder of macular hyperpigmentation which involves mostly in sun exposed areas of the face and neck. Those most affected are women. Multiple factors have been postulated to involve in the etiology and pathogenesis of melasma including pregnancy, oral contraceptives, genetics, sun exposure, cosmetics and race. We have conducted a clinical trial utilizing all trans-retinoic acid (tretinoin, Retin-A) cream 0.1% q pm and hydroquinone lotion 3% (Melanex) applied every morning in Korean women with melasma. Our study patients demonstrated all three clinical patterns common to melasma: centrofacial, malar and mandibular. Wood's light examination was performed on all patients and identified two of the four types of melasma described. Most patients showed epidermal melasma and a few manifested a mixed type. No patients exhibited solely dermal or inapparent type in melasma. With open studies of tretinoin cream and hydroquinone lotion followed by sun screen, we have found significant improvement within 5 months with a few side effects. Histopathologic examination of melasma in the pre-trial biopsies revealed increased pigmentation of the epidermis, dermis or both. In addition, significant alterations of the dermis with solar damage was noted in all melasma patients sampled. Biopsies taken after five months of treatment revealed significant decreases in epidermal pigmentation and improvement of solar damage in the dermis. We reconfirmed that a synergistic mechanism between tretinoin and hydroquinone is responsible for the improvement seen in the female Korean melasma patients from our study.
=============================================================
2.) Mandibular melasma
=============================================================
P R Health Sci J 2000 Sep;19(3):231-4
Mandry Pagan R , Sanchez JL
Department of Dermatology, University of Puerto Rico School of Medicine, San Juan 00936-5067.
[Record supplied by publisher]
Melasma is an acquired symmetrical brown hypermelanosis of the face. Three clinical patterns are recognized, namely centrofacial, malar and mandibular. This study addresses the clinical and histopathological features of ten women with mandibular melasma to determine its relation to other types of melasma. The mean age of the patients was 52 years and the onset of the disease occurred at an average age of 44 years. Sunlight aggravated the pigmentation in all cases. Only one patient was receiving hormonal therapy. Histopathologically, all patients demonstrated severe sundamage and hyperpigmentation of the epidermis. Nine of them had melanophages or melanin in the papillary dermis. We conclude than mandibular melasma may be a clinicopathologic entity different to other types of melasma.
=============================================================
3.) Melasma in men. A clinical and histologic study.
=============================================================
Int J Dermatol 1988 Jan-Feb;27(1):25-7
Vazquez M, Maldonado H, Benmaman C, Sanchez JL
Department of Dermatology, University of Puerto Rico School of Medicine, San Juan.
Melasma is characterized by a facial hypermelanosis of light to dark brown color, being more common in women of Hispanic origin. In this study, 27 men with melasma were evaluated clinically and histologically to compare their features with those of previous studies. Three patterns of localization were recognized, namely, centrofacial, malar, and mandibular. On the basis of Wood's light examination, an epidermal, a dermal, and a mixed type were identified. Epidermal hyperpigmentation only and epidermal and dermal hyperpigmentation were found in histologic analysis of the cases. Significant etiologic factors included exposure to sunlight in 66.6% as well as a familial predisposition in 70.4% of the cases. This study demonstrated that melasma in men shares the same clinicohistologic characteristics as in women, but hormonal factors do not seem to play major significant role.
=============================================================
4.) Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study.
=============================================================
J Am Acad Dermatol 1981 Jun;4(6):698-710
Sanchez NP, Pathak MA, Sato S, Fitzpatrick TB, Sanchez JL, Mihm MC
Melasma is an acquired brown hypermelanosis of the face. Although it is thought that melasma is associated with multiple etiologic factors (pregnancy, gastric, racial, and endocrine), one of the primary causes of its exacerbation appears to be exposure to sunlight. Three patterns of melasma are recognized clinically: (1) a centrofacial pattern, (2) a malar pattern, and (3) a mandibular pattern. Examination of patients with Wood's light (320--400 nm) is useful in classifying the specific type of melasma in correlation with the localization of pigment granules (melanosomes) in the epidermis and dermis. Four types of melasma are described on the basis of Wood's light examination: (1) an epidermal type, (2) a dermal type, (3) a mixed type, and (4) a fourth type, described in patients of dark complexion, in which the lesions, for lack of contrast, are not discernible on Wood's light examination, perhaps due to the increased number of melanosomes in the normal skin of black individuals. Light, histochemical, and electron microscopic studies revealed an increase in number and activity of type-specific melanocytes which appeared to be engaged in increased formation, melanization, and transfer of pigment granules (melanosomes) to the epidermis as well as to the dermis. The melanocyte seems to undergo a functional alteration brought about by a combination of multiple factors, including persistent sun exposure, hormonal factors, and genetic predisposition.
=============================================================
5.) Retrospective study on the clinical presentation and treatment outcome of melasma in a tertiary dermatological referral centre in Singapore.
=============================================================
Singapore Med J 1999 Jul;40(7):455-8
Goh CL, Dlova CN
National Skin Centre, Singapore.
BACKGROUND: This is a retrospective study on the epidemiology of 205 patients with melasma seen in a tertiary dermatological referral centre in Singapore. PATIENTS: The mean age of the 205 patients with melasma was 42.3 years with a female preponderance of 21:1 female to male ratio. There were proportionally more Chinese with melasma than the other races compared to the racial distribution of patients attending our clinic. Ninety percent of our patients had skin type III or IV. The mean age of onset of melasma was 37.6 years. Most sought treatment only 5 years after the appearance of their melasma. Forty-six percent of melasma were light brown, the majority of which were distributed on the malar areas (89%). More than 2/3 had epidermal melasma. Eighty-eight percent had mild localised melasma (occurring on < 20% of the total facial area). Only 26.8% of our patients reported sun exposure, 25 (12.1%) reported pregnancy and 27 (13.1%) reported oral contraceptives as precipitating factors. A positive family history of melasma was observed in 21 (10.2%) patients. Sunscreen forms the backbone in the treatment of melasma in our patients. Most patients were prescribed a sunscreen together with hydroquinone containing bleaching cream (54%) as first line treatment. Patients with epidermal type of melasma responded slightly better to treatment than those with dermal type of melasma (28% experienced > 25% reduction in pigmentation compared to 16% respectively (n.s.)). CONCLUSION: Overall, 53% of our patients experienced some reduction of pigmentation with 28% experiencing > 25% reduction and 7% experiencing > 75% reduction. In 40%, the pigmentation remained stable with treatment. Treatment of melasma remains an enigma. More studies need to be undertaken to improve treatment response to alleviate the psychosocial impact melasma has on the patient.
=============================================================
6.) Usefulness of retinoic acid in the treatment of melasma.
=============================================================
J Am Acad Dermatol 1986 Oct;15(4 Pt 2):894-9
Pathak MA, Fitzpatrick TB, Kraus EW
Melasma is a circumscribed brown macular hypermelanosis of the areas of the face and neck that are exposed to light. Clinical trials with various depigmenting formulations containing hydroquinone were conducted to determine the ideal concentration of hydroquinone, retinoic acid, and corticosteroids for the treatment of melasma. The compounds were tested with and without the concomitant use of topical sunscreen preparations. Based on the results of the trials and our earlier clinical experience, we conclude that treatment of melasma should involve the following: avoidance of sun exposure, constant use of broad-spectrum sunscreens, and topical application of a cream or lotion containing 2% hydroquinone and 0.05% to 0.1% retinoic acid (tretinoin). Patients should suspend use of oral contraceptives and other agents that promote skin pigmentation. The monobenzyl ether of hydroquinone should never be used in melasma therapy.
=============================================================
7.) Topical liquiritin improves melasma.
=============================================================
Int J Dermatol 2000 Apr;39(4):299-301 Related Articles, Books, LinkOut
Amer M, Metwalli M
Department of Dermatology, Zagazig University, Egypt.
Twenty women with a clinical diagnosis of melasma were treated with liquiritin cream on one side of the face and with a vehicle cream on the other side twice daily for 4 weeks. Patients were advised to avoid sun exposure and/or used topical sunscreen during the entire period of treatment. Inclusion criteria included an age range from 18 to 40 years and bilateral and symmetrical idiopathic epidermal melasma. Exclusion criteria included patients with dermal melasma (differentiated by Wood's light), melasma with pregnancy, and patients currently receiving hormone replacement therapy. Melasma pigmentary intensity was rated on a five-point scale in relation to the patient's normal facial skin (1, no difference; 2, slightly more pigmented; 3, moderately more pigmented; 4, markedly more pigmented; and 5, intensely more pigmented). The size of the lesions was measured directly using a millimeter grid scale. Ratings and measurements were made prior to treatment and at each of the follow-up visits (after 2, 4, 6, 8, and 10 weeks). Clinical evaluation was performed at week 4; the overall response was rated as excellent, good, fair, or poor. Color photographs were taken at the start and at week 4 of the study. Side-effects were observed and treated.
=============================================================
8.) Erbium:YAG laser resurfacing for refractory melasma.
=============================================================
Dermatol Surg 1999 Feb;25(2):121-3
Manaloto RM, Alster T
Washington Institute of Dermatologic Laser Surgery, Washington, DC, USA.
BACKGROUND: Melasma is a facial dyspigmentation which is a common complaint in patients with darker skin tones. Many current therapies used for this condition are ineffective and can cause significant adverse effects. OBJECTIVE: The purpose of this study was to evaluate the role of erbium:YAG laser resurfacing in the management of refractory melasma. METHODS: Ten female patients with melasma unresponsive to previous therapy of bleaching creams and chemical peels were included in this study. Full face skin resurfacing using an erbium: YAG laser (2.94 microm) was performed using 5.1-7.6 J/cm2 energy. Clinical evaluations using the Melasma Area and Severity Index (MASI) and melanin reflectance spectrometry measurements were taken preoperatively and at 0.5, 1, 1.5, 3, and 6 weeks and 3, 5, and 6 months postoperatively. Adverse effects after laser resurfacing such as prolonged erythema, infection, and hyperpigmentation were recorded. RESULTS: There was marked improvement of the melasma immediately after laser surgery using the parameters outlined; however, between 3 and 6 weeks postoperatively, all patients exhibited post-inflammatory hyperpigmentation. Decreased MASI and melanin reflectance spectrometry measurement scores were noted after biweekly glycolic acid peels and at the end of 6 months, significant clinical improvement in the melasma was seen compared to the preoperative evaluation. CONCLUSION: Erbium:YAG laser resurfacing effectively improves melasma; however, the almost universal appearance of transient post-inflammatory hyperpigmentation necessitates prompt and persistent intervention. The use of this laser therapy is recommended only for refractory melasma.
=============================================================
9.) Association of melasma with thyroid autoimmunity and other thyroidal abnormalities and their relationship to the origin of the melasma.
=============================================================
J Clin Endocrinol Metab 1985 Jul;61(1):28-31
Lutfi RJ, Fridmanis M, Misiunas AL, Pafume O, Gonzalez EA, Villemur JA, Mazzini MA, Niepomniszcze H
Melasma is localized hyperpigmentation over the forehead, upper lips, cheeks, and chin. In this study, evidence suggesting an association between autoimmune thyroid disorders and melasma and the relationship of thyroid disorders to the origin of melasma is presented. A total of 108 nonpregnant women, aged 20-56 yr, were divided into 2 groups for the purpose of this study: 1) melasma, 84 patients; 2) control group, 24 patients from the Dermatology Clinic matched for age and sex. Microsomal thyroid autoantibodies (MCHA) were sought in all subjects. TRH-TSH tests were performed in patients with melasma and in those women with goiter and/or positive MCHA tests from the control group. Studies were completed with serum T4, T3, and antithyroglobulin antibody (TGHA) measurements in all patients with thyroid abnormalities. In patients with melasma, the frequency of thyroid disorders (58.3%) was 4 times greater than in the control group. The MCHA-negative patients had 1) simple goiter (13.1%), 2) Plummer's disease (2.4%), and 3) TSH hyperresponse to TRH in nongoitrous patients (10.7%). Patients with positive MCHA tests (32.1%) were divided into 2 subgroups. One comprised those women with an apparently normal thyroid gland and thyroid function (n = 7), while the other included all patients with goiter and/or subclinical hypothyroidism (n = 20). Regarding the origin of the melasma, it was found that 70% of women who developed melasma during pregnancy or while using oral contraceptives had thyroid abnormalities compared to 39.4% of patients with idiopathic melasma. Subjects from the control group had a 12.5% incidence of thyroid abnormalities, and only 8.3% had positive MCHA. Estrogen, progesterone, or both could be the triggering factor in the development of melasma in women who have a particular predisposition toward both melasma and thyroid autoimmunity. Patients with idiopathic melasma had a lower frequency of thyroid abnormalities, suggesting that there may be different genetic patterns linked to autoimmune thyroid disease. We conclude that there is a true association between thyroid autoimmunity and melasma, mostly in women whose melasma develops during pregnancy or after ingestion of oral contraceptive drugs.
=============================================================
10.) Topical retinoic acid (tretinoin) for melasma in black patients. A vehicle-controlled clinical trial.
=============================================================
Arch Dermatol 1994 Jun;130(6):727-33
Kimbrough-Green CK, Griffiths CE, Finkel LJ, Hamilton TA, Bulengo-Ransby SM, Ellis CN, Voorhees JJ
Department of Dermatology, University of Michigan Medical Center, Ann Arbor.
BACKGROUND AND DESIGN: Melasma is an acquired, masklike, facial hyperpigmentation. The pathogenesis and treatment of melasma in black (African-American) patients is poorly understood. We investigated the efficacy of topical 0.1% all-trans-retinoic acid (tretinoin) in the treatment of melasma in black patients. Twenty-eight of 30 black patients with melasma completed a 10-month, randomized, vehicle-controlled clinical trial in which they applied either 0.1% tretinoin or vehicle cream daily to the entire face. They were evaluated clinically (using our Melasma Area and Severity Index), colorimetrically, and histologically. RESULTS: After 40 weeks, there was a 32% improvement in the Melasma Area and Severity Index score in the tretinoin treatment group compared with a 10% improvement in the vehicle group. Colorimetric measurements showed lightening of melasma after 40 weeks of tretinoin treatment vs vehicle. Lightening of melasma, as determined clinically, correlated well with colorimetric measurements. Histologic examination of involved skin revealed a significant decrease in epidermal pigmentation in the tretinoin group compared with the vehicle group. Side effects were limited to a mild "retinoid dermatitis" occurring in 67% of tretinoin-treated patients. Among the patients in this study in comparison with comparably recruited white patients, melasma was reported to have begun at a later age and was more likely to be in a malar distribution. CONCLUSIONS: This controlled study demonstrates that topical 0.1% tretinoin lightens melasma in black patients, with only mild side effects.
=============================================================
11.) Melasma in men: a hormonal profile.
=============================================================
J Dermatol 2000 Jan;27(1):64-5
Sialy R, Hassan I, Kaur I, Dash RJ
Department of Dermatology, Venereology & Leprology, Postgraduate Institute of Medical and Research, Chandigarh, India.
Melasma in men is much less common than in women. In the present communication, we evaluated circulating levels of LH, FSH, and testosterone in 15 men with idiopathic melasma. When compared with eleven age matched control men, the circulating LH was significantly higher and testosterone was markedly low in the melasmic men. We conclude that male melasma involves subtle testicular resistance.
12: J Med Assoc Thai 1999 Sep;82(9):868-75 Related Articles, Books, LinkOut
=============================================================
12.) Topical isotretinoin for melasma in Thai patients: a vehicle-controlled clinical trial.
=============================================================
Leenutaphong V, Nettakul A, Rattanasuwon P
Department of Dermatology, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand.
BACKGROUND: Melasma is an acquired hyperpigmentary disorder commonly seen in Orientals. Recently it has been demonstrated that tretinoin (all-trans-retinoic acid) can produce significant clinical improvement of melasma. However, moderate cutaneous side effects (retinoid dermatitis) occurred in a number of patients. OBJECTIVE: To investigate the efficacy of topical 0.05 per cent isotretinoin gel (Isotrex) in the treatment of melasma in Thai patients. METHOD: Thirty patients with moderate to severe melasma entered a 40-week, randomized, vehicle-controlled clinical trial in which they applied either 0.05 per cent isotretinoin gel, or its vehicle base together with a broad spectrum sunscreen (SPF 28) daily to the entire face. They were evaluated clinically (using Melasma Area and Severity Index), and colorimetrically (using our Melasma Area and Melanin Index). RESULTS: After 40 weeks, the average MASI and MAMI scores of the isotretinoin-treated group decreased by 68.2 per cent and 47 per cent respectively, while the corresponding control scores declined 60 per cent and 34 per cent. There was no statistically significant difference between the isotretinoin and vehicle groups. When the MASI and MAMI scores of each visit were compared to their baseline data, a statistically significant reduction of the score was first noted at weeks 4 and 12 respectively. Lightening of melasma, as determined clinically (MASI score), correlated well with pigmentation measurements (MAMI score). Side effects were limited to a mild transient "retinoid dermatitis" occurring in 27 per cent of isotretinoin-treated patients. CONCLUSION: Daily use of broad spectrum sunscreen has a significant lightening effect on melasma in Thai patients. However, there was no statistically significant difference between the isotretinoin and vehicle-treated group.
=============================================================
13.) [Use of a cream based on 20% azelaic acid in the treatment of melasma].
=============================================================
G Ital Dermatol Venereol 1989 Jan-Feb;124(1-2):I-VI
[Article in Italian]
Rigoni C, Toffolo P, Serri R, Caputo R
A 20% azelaic acid base cream (Skinoren-Schering) known in the treatment of acne has been used in melasma. The statistically processed results refer to 39 patients treated for 6 months with 2 applications/die. The reduction in melasma intensity was obtained in all patients bar two whose basal pigmentation situation was already compromised. Overall assessment on a graduated scale in cm evidences, after 6 months of treatment, a mean reduction in pigmentation of 51.3% understood as intensity and surface. The overall judgment of physician and patient on the preparation coincide with some 79% excellent and good on the part of the physician and 85% on the part of the patient. Noteworthy is the absolute absence of sensitisation or leukoderma or any of the other typical side-effects of the other depigmentants available thus far.
=============================================================
14.) The efficacy of a broad-spectrum sunscreen in the treatment of melasma.
=============================================================
Cutis 1983 Jul;32(1):92, 95-6
Vazquez M, Sanchez JL
A double-blind study comparing a broad-spectrum sunscreen agent with its vehicle in the treatment of melasma was performed in fifty-three patients who were concomitantly using a depigmentating solution. In this study, 96.2 percent of those who used the sunscreen agent showed improvement as compared with 80.7 percent of those who used placebo. These results confirm the positive role of sun protection in the treatment of melasma and also establish hydroquinone as a major therapeutic agent in pigmentary disorders.
=============================================================
15.) Actinic lichen planus mimicking melasma. A clinical and histopathologic study of three cases.
=============================================================
J Am Acad Dermatol 1988 Feb;18(2 Pt 1):275-8
Salman SM, Khallouf R, Zaynoun S
Department of Dermatology, American University of Beirut, Lebanon.
Three cases of actinic lichen planus mimicking melasma are presented. Although the clinical similarity to melasma is striking, the histopathologic picture is distinctive. It is suggested that actinic lichen planus be considered in the differential diagnosis of melasma.
Comment in:
J Am Acad Dermatol. 1989 Oct;21(4 Pt 1):815
=============================================================
16.) Glycolic acid peels in the treatment of melasma among Asian women.
=============================================================
Dermatol Surg 1997 Mar;23(3):177-9
Lim JT, Tham SN
National Skin Centre, Singapore.
BACKGROUND: Melasma is a common disorder of facial hyperpigmentation among Asian women. Many modalities of treatment are available but none is satisfactory. OBJECTIVE: This study was undertaken to see if glycolic acid peels are effective and safe in the treatment of melasma and fine facial wrinkling. METHODS: Ten Asian women with moderate to severe melasma were recruited into the study. The women had twice daily applications of a cream containing 10% glycolic acid and 2% hydroquinone (Neostrata AHA Age Spot and Skin Lightening Gel) to both sides of the face, and glycolic acid peels every 3 weeks (20-70%) to one-half of the face using Neostrata Skin Rejuvenation System. All patients had to use a sunblock (SPF 15%). At regular intervals and at the end of 26 weeks (or after eight peels) the degree of improvement of pigmentation and fine facial wrinkling on each side of the face were assessed. Any skin irritation or side effects were also noted. Assessment was by an independent dermatologist, the patients themselves, and the use of the Munsell color chart and photographs. The nonparametric Wilcoxon Rank-Sum test was used for statistical analysis. RESULTS: The melasma and fine facial wrinkling improved on both sides of the face. The side that received glycolic acid peels did better but the results were not statistically significant (P > 0.059). CONCLUSION: A cream containing 10% glycolic acid and 2% hydroquinone (Neostrata AHA Age Spot and Skin Lightening Gel) improved melasma and fine facial wrinkling in Asian women. In combination with glycolic acid peels at 3-week intervals the lightening of melasma is subjectively much better. This improvement does not reach statistical significance and the sample size is small (n = 10).
=============================================================
17.) Endocrinologic profile of patients with idiopathic melasma.
=============================================================
J Invest Dermatol 1983 Dec;81(6):543-5
Perez M, Sanchez JL, Aguilo F
Complete endocrinologic evaluation of 9 women (ages 24-41) with idiopathic melasma (melasma not associated with pregnancy nor ingestion of oral contraceptives) was performed and compared to age- and sex-matched normal controls. Serum cortisol, adrenocorticotropin, plasma immunoreactive alpha and beta melanocyte-stimulating hormones, luteinizing hormone, follicular-stimulating hormone, estradiol and progesterone levels were performed in the basal state. Additionally, total T4, T3RU, FTI, prolactin, 2-h postprandial blood sugar, and 24-h urine for 17-hydroxysteroids and 17-ketosteroids were done and found to be normal. The melasma patients presented statistically significant increased levels of LH (p less than 0.001) and lower levels of serum estradiol (p less than 0.025) than normal controls. It is proposed that these hormonal alterations may represent subclinical evidence of a mild ovarian dysfunction which may underlie the pathogenesis of some cases of idiopathic melasma.
=============================================================
18.) 5-Fluorouracil as an aid in management of acne and melasma.
=============================================================
J Am Acad Dermatol 1981 Jan;4(1):97-8
Milstein HG
Publication Types:
Letter
=============================================================
=============================================================
19.) Topical tretinoin (retinoic acid) improves melasma. A vehicle-controlled, clinical trial.
=============================================================
Br J Dermatol 1993 Oct;129(4):415-21
Griffiths CE, Finkel LJ, Ditre CM, Hamilton TA, Ellis CN, Voorhees JJ
Department of Dermatology, University of Michigan Medical Center, Ann Arbor 48109-0314.
Melasma is a common disorder of cutaneous hyperpigmentation predominantly affecting the faces of women. Little is known about the aetiology of melasma, and treatment is frequently disappointing. Topical tretinoin is of benefit in treating other forms of hyperpigmentation, for example liver spots, and we therefore investigated its effectiveness in melasma. Thirty-eight women completed a randomized, vehicle-controlled study, in which they applied 0.1% tretinoin (n = 19) or vehicle cream (n = 19) once daily to the face for 40 weeks. At the end of treatment 13 (68%) of 19 tretinoin-treated patients were clinically rated as improved or much improved, compared with 1 (5%) of 19 in the vehicle group (P = 0.0006). Significant improvement first occurred after 24 weeks of tretinoin treatment. Colorimetry (an objective measure of skin colour) demonstrated a 0.9 unit lightening of tretinoin-treated melasma and a 0.3 unit darkening with vehicle (P = 0.01); these results correlated with clinical lightening (r = 0.55, P = 0.0005). Histologically, epidermal pigment was reduced 36% following tretinoin treatment, compared with a 50% increase with vehicle (P = 0.002). Reduction in epidermal pigment also correlated with clinical lightening (r = -0.41, P = 0.01). Moderate cutaneous side-effects of erythema and desquamation occurred in 88% of tretinoin-treated and 29% of vehicle-treated patients. Topical 0.1% tretinoin produces significant clinical improvement of melasma, mainly due to reduction in epidermal pigment, but improvement is slow.
=============================================================
20.) Topical tretinoin, hydroquinone, and betamethasone valerate in the therapy of melasma.
=============================================================
Cutis 1979 Feb;23(2):239-41
Gano SE, Garcia RL
Twenty adult female patients with melasma were followed over a ten week clinical trial in which a combination of depigmenting agents was used daily. Past clinical experience and objective assessment point to enhanced efficacy of this simple depigmenting combination. Certainly, most of depigmenting agents at our command to date have been relatively ineffective. Even this new combination is not the final answer. The purpose of this study is to provide the clinician with a simple yet effective and readily accessible combination of commercially-formulated and available depigmentary agents. A stable combination in a single vehicle with greater efficacy remains to be perfected.
=============================================================
21.) Melasma of the forearms.
=============================================================
Australas J Dermatol 1997 Feb;38(1):35-7
O'Brien TJ, Dyall-Smith D, Hall AP
Department of Dermatology, The Geelong Hospital, Australia.
Melasma of the forearms seems to be a relatively common sign which is, to our knowledge, not reported in the literature. It seems that it may be more common in older patients and especially in postmenopausal women on supplementary oestrogen. The pigmentary change is macular and may be confluent or speckled. Like facial chloasma there is a sharp line of demarcation at the margins. In some, there seems to be an element of erythema.
=============================================================
22.) Treatment of melasma using kojic acid in a gel containing hydroquinone and glycolic acid.
=============================================================
Dermatol Surg 1999 Apr;25(4):282-4
Lim JT
National Skin Care Center, Singapore.
BACKGROUND: Melasma is difficult to clear. Many agents have been used, such as hydroquinone, and glycolic acid and glycolic acid peels, kojic acid, a tyrosinase inhibitor in the fungus Aspergilline oryzae. OBJECTIVE: To see if the addition of 2% kojic acid in a gel containing 10% glycolic acid and 2% hydroquinone will improve melasma further. METHODS: Forty Chinese women with epidermal melasma were treated with 2% kojic acid in a gel containing 10% glycolic acid and 2% hydroquinone on one half of the face. The other half was treated with the same application but without kojic acid. The side receiving the kojic acid was randomized. Determination of efficacy was based on clinical evaluation, photographs and self-assessment questionnaires at 4 weekly intervals until the end of the study at 12 weeks. The non-parametric Wilcoxon's rank sum test was used for statistical analysis. RESULTS: All patients showed improvement in melasma on both sides of the face. The side receiving the kojic acid did better. More than half of the melasma cleared in 24/40 (60%) patients receiving kojic acid compared to 19/40 (47.5%) patients receiving the gel without kojic acid. In 2 patients, there was complete clearance of melasma, and this was on the side where kojic acid was used. Side effects include redness, stinging, and exfoliation. These were seen on both sides of the face, and they settled by the third week. CONCLUSION: The addition of kojic acid to a gel containing 10% glycolic acid and 2% hydroquinone further improves melasma.
=============================================================
23.) [Melasma in pregnancy: reduction of its appearance with the use of a broad-spectrum photoprotective agent].
=============================================================
Med Cutan Ibero Lat Am 1987;15(3):199-203
[Article in Spanish]
Abarca J, Odilla Arrollo C, Blanch S, Arellano G
Servicio de Dermatologia, Hospital J. J. Aguirre, Santiago, Chile.
65 pregnant women distributed in two groups, by a double-blind method received a placebo or a sunscreen cream (Pabafil SPF 10, with absorption range from 290 to 360 nm) for daily use on face during the second quarter of their pregnancy in summer time. In 30 patients "with optimum fulfillment" in the products application (16 with placebo and 14 with sunscreen cream) the melasma appearances were significantly lower in those with sunscreen application. In subgroups of the total number of pregnant women, with similar proportion of patients with placebo and sunscreen, the melasma appearances were significantly lower in skin types I-II, and in those that used cosmetics (versus those that did not). No differences were observed in subgroups by age, parity, and with or without history of previous melasma.
=============================================================
24.) Melasma. Etiologic and therapeutic considerations.
=============================================================
Arch Dermatol 1995 Dec;131(12):1453-7
Grimes PE
Division of Dermatology, King-Drew Medical Center, Los Angeles, Calif.
BACKGROUND: Melasma is a common acquired symmetric hypermelanosis characterized by irregular light- to gray-brown macules and patches involving sun-exposed areas of skin. Etiologic factors in the pathogenesis of melasma include genetic influences, exposure to UV radiation, pregnancy, hormonal therapies, cosmetics, phototoxic drugs, and antiseizure medications. OBSERVATIONS: Melasma is often a therapeutically challenging disease, and current treatments include hypopigmenting agents, chemical peels, and lasers. Hypopigmenting agents include phenolic and nonphenolic derivatives. Phenolic agents include hydroquinone and hydroquinone combination preparations. Despite controversies regarding the issue of hydroquinone-induced ochronosis, hydroquinone remains the most effective topically applied bleaching agent approved by the Food and Drug Administration for the treatment of melasma. Nonphenolic bleaching agents include tretinoin and azelaic acid. Superficial, medium, and deep chemical peels are more often used in lighter-complexioned patients. Such peels should be used with caution in blacks. Although lasers have demonstrated significant efficacy in the treatment of a variety of hyperpigmentary disorders, their precise efficacy and place in the therapy of melasma have yet to be established. CONCLUSIONS: In the hierarchy of therapies for melasma, the treating physician must consider the devastating psychosocial impact of pigmentary imperfections within the realm of the benefits and risks associated with each treatment.
=============================================================
25.) Double-blind comparison of azelaic acid and hydroquinone in the treatment of melasma.
=============================================================
Acta Derm Venereol Suppl (Stockh) 1989;143:58-61
Verallo-Rowell VM, Verallo V, Graupe K, Lopez-Villafuerte L, Garcia-Lopez M
Department of Dermatology, Makati Medical Center, Manila, Philippines.
Melasma is a macular hypermelanosis of the sun-exposed areas of the face and neck. The clinical efficacy of azelaic acid (20%) and hydroquinone creams (2%) in the treatment of this benign pigmentary disorder was compared in a randomized, double-blind study with 155 patients of Indo-Malay-Hispanic origin. The creams were applied twice daily. A broad spectrum sunscreen was used concomitantly. Over a period of 24 weeks, 73% of the azelaic acid patients, compared with 19% of the hydroquinone patients, had good to excellent overall results, as measured by the reduction of melasma pigmentary intensity and lesion size. Transient mild to moderate irritant reactions were initially seen with both test drugs.
=============================================================
26.) N-acetyl-4-S-cysteaminylphenol as a new type of depigmenting agent for the melanoderma of patients with melasma.
=============================================================
Arch Dermatol 1991 Oct;127(10):1528-34
Jimbow K
Division of Dermatology and Cutaneous Sciences, Faculty of Medicine, University of Alberta, Edmonton, Canada.
BACKGROUND AND DESIGN.--Melasma is a difficult medical problem to treat. Hydroquinone is administered to many patients, but it is unstable and local irritation and dermatitis may develop after a prolonged use at a high concentration. This study introduces a new depigmenting agent, N-acetyl-4-S-cysteaminylphenol, for better management of melanoderma in patients with melasma. RESULTS.--Our study, based on a retrospective observation of 12 patients using 4% N-acetyl-4-S-cysteaminylphenol in oil-in-water emulsion, showed a complete loss (8%), a marked improvement (66%), or a moderate improvement (25%) of melasma lesions. Visible changes of melanoderma can be seen in 2 to 4 weeks after daily topical application. This depigmentation was associated with a decrease in the number of functioning melanocytes and in the number of melanosomes transferred to keratinocytes. N-acetyl-4-S-cysteaminylphenol is the tyrosinase substrate, and, on exposure to tyrosinase, it formed a melanin-like pigment. CONCLUSIONS.--A phenolic thioether, N-acetyl-4-S-cysteaminylphenol, is a new type of depigmenting agent for the better management of melasma. It is much more stable and less irritating to the skin than hydroquinone, and it is specific to melanin-synthesizing cells.
=============================================================
27.) Treatment of melasma (chloasma) by local application of a steroid cream.
=============================================================
Dermatologica 1975;151(6):349-53
Neering H
15 patients with melasma were treated with betamethasone 17-valerate in a cream base containing DMSO. One patient with secondary pigmentation was also entered in the trial. In nine patients results were favourable and in three results were moderate. This effect could be ascribed to the steroid.
=============================================================
28.) Hormonal milieu in the maintenance of melasma in fertile women.
=============================================================
J Dermatol 1998 Aug;25(8):510-2
Hassan I, Kaur I, Sialy R, Dash RJ
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Melasma is a specific type of facial hyperpigmentation seen in women taking oral contraceptives, in non-pregnant women who have not used oral contraceptives, and in some pregnant women during the progression of gestation, but rarely in men. Circulating LH, FSH, PRL, and E2-17 beta on day 5, 7, 9, and 11 of the menstrual cycle and progesterone (P) on day 17, 19, and 21 were measured in thirty-six ovulating women with melasma (study group) age 25-35 years and twelve healthy controls (control group). Twenty-seven subjects in the study group had normal pregnancies; 9 others were married or single and had no history of contraceptive pill use. Higher levels of FSH on day 7 (p < 0.05); E2-17 beta on 5, 7, 9 (p < 0.05) and LH on day 9 (p < 0.002) were observed in the study group than in the control group. There were no significant differences between the LH/FSH ratio in the two groups. Serum PRL was lower on day 9 in the study group (p < 0.05) than in the control group. Serum P was similar in the patients and the controls. These findings indicate a possible role of high E2-17 beta in the maintenance of melasma.
=============================================================
29.) Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser.
=============================================================
J Dermatol Surg Oncol 1994 Sep;20(9):592-7
Taylor CR, Anderson RR
Wellman Laboratories of Photomedicine, Massachusetts General Hospital, Harvard Medical School, Boston 02114.
BACKGROUND. Melasma and postinflammatory pigmentation are cosmetic problems with limited options for treatment. OBJECTIVE. To determine whether selective photothermolysis of pigmented cells by Q-switched ruby laser treatment would produce clinical benefit in these disorders. METHODS. Eight subjects with melasma or postinflammatory hyperpigmentation refractory to traditional treatments were treated with Q-switched ruby laser pulses (694 nm, 40 nanoseconds) at fluences of 15-7.5 J/cm2, and followed. Histology was obtained before and after treatment. RESULTS. Regardless of fluence, no permanent improvement and, in some cases, darkening was seen in each type of lesion. Except for small depression at high fluences in black patients, there were no textural changes after healing. Immediately after treatment, there was epidermal and dermal injury, with extracellular melanin. Several months later, epidermal pigmentation had returned to baseline and dermal macrophages were apparently focally increased. CONCLUSIONS. The Q-switched ruby laser by itself does not provide an effective treatment for refractory melasma or postinflammatory hyperpigmentation.
=============================================================
30.) The combination of glycolic acid and hydroquinone or kojic acid for the treatment of melasma and related conditions.
=============================================================
Dermatol Surg 1996 May;22(5):443-7
Garcia A, Fulton JE
BACKGROUND: Melasma continues to be a difficult problem. Although the cause is genetic, the condition is aggravated with sunlight, birth control pills, and pregnancy. Although hydroquinone is effective and has been available for years, a new product, kojic acid, has the advantage of being pharmaceutically more stable and, also, a tyrosinase inhibitor. OBJECTIVE: To evaluate on melasma and related conditions two similar formulations of glycolic acid/hydroquinone and glycolic acid/kojic acid. The therapeutic index of the two formulations is examined. METHODS: Thirty-nine patients were treated with kojic acid on one side of the face and hydroquinone in a similar vehicle on the other side of the face. The results were documented by a clinical investigator and with Wood's light examination combined with ultraviolet light photography. RESULTS: Fifty-one percent of the patients responded equally to hydroquinone and kojic acid. Twenty-eight percent had a more dramatic reduction in pigment on the kojic acid side; whereas 21% had a more dramatic improvement with the hydroquinone formulation. These results were not statistically different. The kojic acid preparation was more irritating. CONCLUSION: Both glycolic acid/kojic acid and glycolic acid/hydroquinone topical skin care products are highly effective in reducing the pigment in melasma patients. Both formulations should be available to the dermatologist to satisfy the patient's preferences.
=============================================================
31.) Intermittent therapy for melasma in Asian patients with combined topical agents (retinoic acid, hydroquinone and hydrocortisone): clinical and histological studies.
=============================================================
J Dermatol 1998 Sep;25(9):587-96
Kang WH, Chun SC, Lee S
Department of Dermatology, Ajou University School of Medicine, Suwon, Korea.
Melasma is a common problem in Asians, but treatments have not been satisfactory. In the present study, we evaluated the efficacy of a new formula containing 0.1% tretinoin, 5% hydroquinone, and 1% hydrocortisone (RHQ) in Korean patients with melasma. Twenty-five Korean females with therapy recalcitrant melasma applied RHQ on their faces for 4 months and were evaluated before and 4 weeks after treatment clinically and histologically. They were also evaluated clinically 4 months after treatment. To minimize unavoidable side effects (erythema or peeling), we applied RHQ twice a week instead of the usual daily application. However, we obtained clinical and histological results comparable to other reports from white populations. Statistically significant depigmentation in clinical and histological studies and increased subepidermal collagen synthesis were observed in this study. These effects were seen as early as 4 weeks after treatment with RHQ. We used mMASI scoring, a modified version of the original MASI, to quantify the effects of RHQ more objectively and easily.
=============================================================
32.) Melanin hyperpigmentation of skin: melasma, topical treatment with azelaic acid, and other therapies.
=============================================================
Cutis 1996 Jan;57(1 Suppl):36-45
Breathnach AS
Sherrington School of Physiology, UMDS, University of London, England, United Kingdom.
Clinical studies of patients with melasma have shown that topical 20 percent azelaic acid is superior to 2 percent hydroquinone and as effective as 4 percent hydroquinone, without the latter's undesirable side effects. Tretinoin appears to enhance this effect of azelaic acid. Azelaic acid with tretinoin caused more skin lightening after three months than azelaic acid alone, and a higher proportion of excellent responders at the end of treatment. The effect of azelaic acid can be attributed to its ability to inhibit the energy production and/or DNA synthesis of hyperactive melanocytes, and partially to its antityrosinase activity. This may also account for the beneficial effect on postinflammatory hyperpigmentation. Destruction of malignant melanocytes by a combination of the same activities, enhanced by the greater permeability of tumoral cells to azelaic acid, may account for the clinical effects of azelaic acid observed in lentigo maligna and individual lesions of primary melanoma.
=============================================================
33.) The treatment of melasma. 20% azelaic acid versus 4% hydroquinone cream.
=============================================================
Int J Dermatol 1991 Dec;30(12):893-5
Balina LM, Graupe K
Department of Dermatology, Argerich Hospital, Buenos Aires, Argentina.
The efficacy of 20% azelaic acid cream and 4% hydroquinone cream, both used in conjunction with a broad-spectrum sunscreen, against melasma was investigated in a 24-week, double-blind study with 329 women. Over the treatment period the azelaic acid cream yielded 65% good or excellent results; no significant treatment differences were observed with regard to overall rating, reduction in lesion size, and pigmentary intensity. Severe side effects such as allergic sensitization or exogenous ochronosis were not observed with azelaic acid.
=============================================================
34.) Treatment of melasma with Jessner's solution versus glycolic acid: a comparison of clinical efficacy and evaluation of the predictive ability of Wood's light examination.
=============================================================
J Am Acad Dermatol 1997 Apr;36(4):589-93
Lawrence N, Cox SE, Brody HJ
Department of Dermatologic Surgery, University of Dentistry and Medicine New Jersey Cooper Hospital/UMC, Marlton, USA.
BACKGROUND: Melasma can be resistant to topical therapy. OBJECTIVE: Our purpose was to evaluate the efficacy of superficial peels in conjunction with topical tretinoin and hydroquinone in patients with melasma and to evaluate the ability of Wood's light examination to predict response to treatment. METHODS: We measured increased light reflectance in melasma areas with a colorimeter. Clinical observations were scored through an index designed to weigh numerically homogeneity, intensity of color, and area of melasma. RESULTS: Colorimetric analysis showed an average lightening of 3.14 +/- 3.1 on the glycolic acid-treated side and 2.96 +/- 4.84 on the Jessner's solution-treated side. There was no statistically significant difference between the right and left. There was an overall decrease in melasma area and severity of 63%. CONCLUSION: Superficial peels hasten the effects of topical therapy in melasma. Wood's light examination did not help predict response to treatment.
=============================================================
35.) The effect of topical tretinoin on the photodamaged skin of the Japanese.
=============================================================
Tohoku J Exp Med 1993 Feb;169(2):131-9
Tadaki T, Watanabe M, Kumasaka K, Tanita Y, Kato T, Tagami H, Horii I, Yokoi T, Nakayama Y, Kligman AM
Department of Dermatology, Tohoku University School of Medicine, Sendai.
Fifteen middle aged or elderly patients with chronic solar damage of the skin, eight patients with melasma and three patients with xeroderma pigmentosum were treated with topical tretinoin for 6 months. There was a significant improvement in fine surface lines in periorbital region, but no significant improvement was observed in deep furrows. No significant change was induced in melasma despite the improvement in smoothness of the skin surface. Global improvement was also seen in one patient with xeroderma pigmentosum. With regard to the functions of the stratum corneum that was assessed on the flexor surface of the forearms, values of water content as well as transepidermal water loss were found to increase one month after start of the application of tretinoin cream. On the other hand, there was no significant change in the amino acid content of the stratum corneum when measured after 4 months of the treatment. It is concluded that tretinoin cream is capable of partly reversing fine surface lines in photodamaged facial skin of the Japanese. However the irritation induced by 0.1% tretinoin cream was unexpectedly severe in the Japanese as compared to that reported in Caucasians.
=============================================================
36.) Combination treatment of melasma with pulsed CO2 laser followed by Q-switched alexandrite laser: a pilot study.
=============================================================
Dermatol Surg 1999 Jun;25(6):494-7
Nouri K, Bowes L, Chartier T, Romagosa R, Spencer J
Department of Dermatology and Cutaneous Surgery, University of Miami School of Medicine, Florida, USA.
BACKGROUND: Melasma is very difficult to treat and often refractory to treatment with topical creams and pigmented-lesion lasers. OBJECTIVE: Pulsed CO2 laser alone is compared with the combination of pulsed CO2 laser followed by Q-switched alexandrite laser in the treatment of dermal-type melasma. This combination is proposed to be effective by first destroying the abnormal melanocytes with the pulsed CO2 laser and then selectively eliminating the dermal melanin with the alexandrite laser. METHODS: Four patients were randomly chosen for each treatment arm. There were multiple follow-up visits for examination by an objective blinded investigator. RESULTS: All patients in the combination laser group showed complete resolution, and two patients in the CO2 laser only group had peripheral hyperpigmentation in the long-term follow-up evaluation. CONCLUSION: These laser therapies are safe, as there was no scarring and no infection. The combination laser therapy was highly effective in removing the hyperpigmentation and all patients in this group showed complete resolution without any peripheral hyperpigmentation.
=============================================================
37.) The use of chemical peelings in the treatment of different cutaneous hyperpigmentations.
=============================================================
Dermatol Surg 1999 Jun;25(6):450-4
Cotellessa C, Peris K, Onorati MT, Fargnoli MC, Chimenti S
Department of Dermatology, University of L'Aquila, Italy.
BACKGROUND: Several chemical agents including hydroquinone, retinoic acid, and azelaic acid are currently used in the treatment of cutaneous hyperpigmentations. Recently chemical peelings with kojic acid, glycolic acid, and trichloroacetic acid, either alone or in combination, have been introduced for treatment of hyperpigmentations. OBJECTIVE: The purpose of our study was to evaluate the efficacy of trichloroacetic acid as well as glycolic acid associated with kojic acid in the treatment of cutaneous hyperpigmentations. METHODS: Twenty patients with diffuse melasma were treated with a solution composed of 50% glycolic acid and 10% kojic acid whereas 20 patients with localized hyperpigmentations (lentigo) were treated with 15%-25% trichloroacetic acid. RESULTS: Complete regression of diffuse melasma was observed in 6 of 20 patients (30%), a partial regression in 12 of 20 patients (60%), and no regression in 2 of 20 patients (10%) treated with 50% glycolic acid and 10% kojic acid. Complete regression of localized hyperpigmentations was observed in 8 of 20 patients (40%), a partial regression in 10 of 20 patients (50%), and no regression in 2 of 20 patients (10%) treated with 15-25% trichloroacetic acid. CONCLUSIONS: Based on our findings, both peelings can be considered effective in the treatment of cutaneous hyperpigmentations.
=============================================================
38.) Glycolic acid peels for the treatment of wrinkles and
photoaging.
=============================================================
J Dermatol Surg Oncol (United States), Mar 1993, 19(3) p243-6
AUTHOR(S): Moy LS; Murad H; Moy RL
ABSTRACT: BACKGROUND. Glycolic acid is an alpha hydroxyacid that is useful as a chemical peeling agent. OBJECTIVE. To discuss the techniques using glycolic acid to remove actinic keratoses, fine wrinkles, lentigines, melasma, and seborrheic keratoses. METHOD. Applied in a carefully timed manner, the depth of penetration can be titrated by the timed duration of application of acid on the skin. Chemical peels are left on the skin for 3 to 7 minutes for most patients. For ideal results, the chemical peel can be repeated 3 to 4 times. RESULT. Glycolic acid can easily be used to peel skin of all skin types with minimal risk. CONCLUSION. We have found glycolic acid can be an ideal adjunct to other cosmetic modalities such as soft tissue augmentation.
=============================================================
39.) A possible mechanism of action for azelaic acid in the human epidermis.
=============================================================
ARTICLE SOURCE: Arch Dermatol Res (Germany, West), 1990, 282(3) p168-71
AUTHOR(S): Schallreuter KU; Wood JW
ABSTRACT: Azelaic acid, and other saturated dicarboxylic acids (C9-C12), are shown to be competitive inhibitors of tyrosinase (KI azelaic acid = 2.73 X 10(-3) M) and of membrane-associated thioredoxin reductase (KI azelaic acid = 1.25 X 10(-5) M). The monomethyl ester of azelaic acid does not inhibit thioredoxin reductase, but it does inhibit tyrosinase, although double the concentration is necessary compared with azelaic acid (KI azelaic acid monomethyl ester = 5.24 X 10(-3) M). Neither azelaic acid nor its monomethyl ester inhibit tyrosinase when catechol is used as a substrate instead of L-tyrosine. Therefore, the weak inhibitory action of azelaic acid on tyrosinase appears to be due to the competition of a single carboxylate group on this inhibitor for the alpha-carboxylate binding site of the L-tyrosine substrate on the enzyme active site. Based on the inhibitor constant on tyrosinase, at least cytotoxic levels of azelaic acid would be required for the direct inhibition of melanin biosynthesis in melanosomes if this mechanism is responsible for depigmentation in the hyperpigmentation disorders lentigo maligna and melasma. Alternatively only 10(-5) M azelaic acid is required to inhibit thioredoxin reductase. This enzyme is shown to regulate tyrosinase through a feedback mechanism involving electron transfer to intracellular thioredoxin, followed by a specific interaction between reduced thioredoxin and tyrosinase. Furthermore, the thioredoxin reductase/thioredoxin system is shown to be a principal electron donor for the ribonucleotide reductases which regulates DNA synthesis.(ABSTRACT TRUNCATED AT 250 WORDS).
=============================================================
40.) A new bleaching protocol for hyperpigmented skin lesions with a high concentration of all-trans retinoic acid aqueous gel.
=============================================================
Aesthetic Plast Surg 1999 Jul-Aug;23(4):285-91
Yoshimura K, Harii K, Aoyama T, Shibuya F, Iga T
Department of Plastic and Reconstructive Surgery, University of Tokyo, Japan.
A new bleaching protocol for skin hyperpigmentation with a higher concentration of all-trans retinoic acid (atRA) aqueous gel than those commercially available is introduced. AtRA aqueous gel (0.1%) was applied topically twice a day along with 4% hydroquinone, 7% lactic acid ointment to oriental patients with hyperpigmented lesions such as senile lentigines, melasma, and postinflammatory hyperpigmentation. The clinical results of 39 patients treated with 0.1% atRA aqueous gel were compared to those of 22 patients treated with 0.1% atRA hydrophilic ointment. Better clinical results and subjective satisfaction were obtained through a significantly shorter period of treatment with 0.1% atRA aqueous gel than with 0. 1% atRA hydrophilic ointment, although side effects such as erythema and irritation were seen at a higher frequency. It is suggested that our bleaching protocol with a high concentration of atRA aqueous gel in combination with hydroquinone and lactic acid has a strong bleaching ability and a potential as a standard therapy for various kinds of skin lesions with hyperpigmentation.
=============================================================
41.) Experience with a strong bleaching treatment for skin hyperpigmentation in Orientals.
=============================================================
Plast Reconstr Surg 2000 Mar;105(3):1097-108; discussion 1109-10
Yoshimura K, Harii K, Aoyama T, Iga T
Department of Plastic, Reconstructive, and Aesthetic Surgery, University of Tokyo, Japan. [email protected]
Although a variety of topical treatments have been used for skin hyperpigmentation, the effectiveness of each varies after prolonged treatment. In this study, 136 Oriental patients who were followed up for more than 12 weeks were analyzed. The treatment protocol was composed of two steps: bleaching (2 to 6 weeks) and healing (2 to 6 weeks); 0.1% to 0.4% all-trans retinoic acid aqueous gel was originally prepared and applied concomitantly with hydroquinone-lactic acid ointment for bleaching. After obtaining sufficient improvement of the hyperpigmentation, a corticosteroid was applied topically with hydroquinone and ascorbic acid for healing. Improvement was evaluated with a narrow-band reflectance spectrophotometer. The results were successful in more than 80 percent of cases of senile lentigines and postinflammatory hyperpigmentations, especially on the face. Sixty percent of cases of nevus spilus were also successfully treated. Although the transient adverse effects of this treatment may be more severe than conventional treatment, this strong bleaching protocol improves a variety of hyperpigmented lesions, including nevus spilus, with a higher success rate and a shorter treatment period than conventional protocols.
=============================================================
42.) Injection of all-trans retinoic acid for treatment of thin wrinkles.
=============================================================
Aesthetic Plast Surg 1997 May-Jun;21(3):196-204
Personelle J, De Campos S, Ruiz Rd, Ribeiro GQ
The authors propose a treatment to improve skin texture and to decrease thin wrinkles and creases. The treatment is based on the use of 0.1% all-trans retinoic acid intradermic injections (with biopresence of 0.02%) combined with topic cream, immediately followed by 340 Nm blue light skin exposure. These procedures determine the retinoic binding protein stabilization that provides the acid intracellular penetration with its subsequent effects. An average of 10 sessions, once a week was required.
=============================================================
43.) Embryotoxicity and teratogenicity of topical retinoic acid.
=============================================================
Skin Pharmacol 1993;6 Suppl 1:35-44
Nau H
Institute of Toxicology and Embryopharmacology, Free University of Berlin, FRG.
All-trans-retinoic acid is a potent developmental toxicant in all species examined. The teratogenic risk of topical all-trans-retinoic acid is reviewed. Experimental studies are limited because of the high maternal toxicity, including skin irritation, with doses below those resulting in significant teratogenic response with other application routes, such as oral application. The maximal systemic availability reported for transdermal exposure of all-trans-retinoic acid was 5-6% in the rat, 9.6% in the monkey (48% with dermatitic skin) and 5-7% in the human. Oral administration of threshold teratogenic doses of all-trans-retinoic acid (6 mg/kg/day) to Wistar rats and Swiss hare rabbits resulted in embryonic area under the concentration time curve levels (approximately 1,000 ng.h/g) which were 2- to 4-fold higher than the endogenous all-trans-retinoic acid levels; corresponding maternal plasma area under the concentration time curve values were 98 and 321 ng.h/ml in rat and rabbit, respectively. The 4-oxo-metabolite was also found in maternal plasma and embryo. Large, controlled studies on the possible developmental toxicity of topical all-trans-retinoic acid in the human are not available. Isolated case reports appeared in the literature claiming teratogenic outcome resembling effects after oral isotretinoin use or those observed in experimental studies with oral or parenteral all-trans-retinoic acid administration. The dose absorbed from daily cosmetic or therapeutic application of all-trans-retinoic acid is expected to be below 0.015 mg/kg, which is at least 30-fold lower than the lowest teratogenic dose of isotretinoin in the human. Topical all-trans-retinoic acid application did not appreciably alter endogenous plasma retinoid levels. The influence of nutrition, diurnal variation and in particular oral vitamin A supplements are more important determinants of plasma retinoic acid compounds than topical all-trans-retinoic acid. These results imply a low risk of therapeutic or cosmetic application of topical all-trans-retinoic acid. However, the highly specific spatial and temporal distribution of binding proteins and nuclear receptors in the embryo suggests that even small alterations in endogenous levels of all-trans-retinoic acid in the embryo may alter crucial developmental processes such as morphogenes; this aspect should be further investigated.
=============================================================
44.) The safety and efficacy of salicylic acid chemical peels in darker racial-ethnic groups.
=============================================================
Dermatol Surg 1999 Jan;25(1):18-22
Grimes PE
Vitiglio & Pigmentation Institute of Southern California, Los Angeles, USA.
BACKGROUND: There is a dearth of published data regarding chemical peels in darker racial-ethnic groups. OBJECTIVE: The purpose of the present investigation was to assess the clinical efficacy and safety of a new superficial salicylic acid peel in individuals of skin types V and VI. METHODS: Twenty-five patients were included in this pilot investigation. Nine had acne vulgaris, 5 had post-inflammatory hyperpigmentation, 6 had melasma, and 5 had rough, oily skin with enlarged pores. The patients were pre-treated for 2 weeks with hydroquinone 4% prior to undergoing a series of five salicylic acid chemical peels. The concentrations of salicylic acid were 20% and 30%. The peels were performed at 2 week intervals. RESULTS. Moderate to significant improvement was observed in 88% of the patients. Minimal to mild side effects occurred in 16%. CONCLUSION: The results of this study suggest that superficial salicylic acid peels are both safe and efficacious for treatment of acne vulgaris, oily skin, textural changes, melasma, and post-inflammatory hyperpigmentation in patients with skin types V and VI.
=============================================================
45.) The combination of 2% 4-hydroxyanisole (Mequinol) and 0.01% tretinoin is effective in improving the appearance of solar lentigines and related hyperpigmented lesions in two double-blind multicenter clinical studies.
=============================================================
J Am Acad Dermatol 2000 Mar;42(3):459-67
Fleischer AB, Schwartzel EH, Colby SI, Altman DJ
Wake Forest University School of Medicine, Winston-Salem, North Carolina, USA.
BACKGROUND: Solar lentigines are a chronic condition of the aging population resulting from years of cumulative sun exposure. A topical treatment that is both safe and effective would be welcome and useful. Combinations of therapeutic agents are often used and allow synergy of mechanisms with tolerability. A tyrosinase inhibitor in use in Europe, 4-hydroxyanisole (Mequinol), and the retinoid tretinoin have been used singly as depigmenting agents. OBJECTIVE: The efficacy and safety of the combination product of 2% 4-hydroxyanisole (4HA [mequinol]) /0.01% tretinoin solution (tradename Solage) were evaluated in two phase III, randomized, controlled, double-blind trials. METHODS: Subjects were randomized to treatment with 4HA/tretinoin solution, one of the active components (4HA or tretinoin), or vehicle. Subjects applied the test solution with a wand applicator twice daily to all solar lentigines and related hyperpigmented lesions on the face, forearms, and backs of hands for up to 24 weeks. Trial 1 had a 24-week no-treatment regression phase and trial 2 had a 4-week no-treatment regression phase. Information collected included clinical assessments of Target Lesion Pigmentation, Physician's Global Assessment of Improvement/Worsening, an Assessment of Overall Cosmetic Effect, and a Subject's Self-Assessment Questionnaire. RESULTS: The 4HA/tretinoin combination was clinically superior to each of its active components and to the vehicle in the treatment of solar lentigines. At the end of treatment, in trial 1 and trial 2, 4HA/tretinoin was statistically superior to each of its active components and vehicle on the forearms and face (P </=.03), except versus tretinoin on the face in trial 2 (P =.2). In trial 2, a trend toward greater efficacy of 4HA/tretinoin over tretinoin on the face was demonstrated at the end of treatment (P =.2), which was also increasingly evident at the end of the 4-week follow-up (P =.06). Most skin-related adverse events were mild and were similar for both the 4HA/tretinoin and tretinoin treatment groups. CONCLUSION: For the treatment of solar lentigines and related hyperpigmented lesions, the topical combination product containing 2% 4HA/0.01% tretinoin solution is well tolerated and superior to either active component.
=============================================================
46.) Combination of 4-hydroxyanisole and all-trans retinoic acid produces synergistic skin depigmentation in swine.
=============================================================
J Invest Dermatol 1993 Aug;101(2):145-9
Nair X, Parab P, Suhr L, Tramposch KM
Bristol-Myers Squibb Co., Pharmaceutical Research Institute, Buffalo, New York 14213.
A combination of 4-hydroxyanisole (4HA) and all-trans retinoic acid (TRA) was found to synergistically cause moderate to complete depigmentation of Yucatan swine skin. Two hyperpigmentation models were used: Natural dark-skinned swine, a potential model for melasma-like disorders, and ultraviolet light-stimulated hyperpigmentation, a model of solar lentigines. Test materials were applied twice daily, 5 d/week, to dorsal flank skin. Application sites were graded at weekly intervals for skin color using a 0 to 4 grading scale. After 8 weeks of treatment of naturally dark swine skin, a combination of 2% 4HA and 0.01% TRA produced grade 2 hypopigmentation (definite but moderate hypopigmentation). In contrast, 2% 4HA alone or 0.01% TRA alone did not produce significant hypopigmentation. After cessation of treatment, the 4HA/TRA-treated sites reverted to normal color within 7-12 weeks. The 4HA/TRA combination completely reversed the hyperpigmentation induced by ultraviolet light after 8 weeks of treatment. In vitro skin-penetration studies using hairless mouse and human skin show that skin penetration of 4HA was not significantly affected by adding 0.01% TRA. These data suggest that the observed synergy is not due to enhanced bioavailability of 4HA. We have demonstrated that combining low concentrations of 4HA and TRA results in effective skin lightening without causing irreversible depigmentation and with minimal local skin irritation.
=============================================================47.) [Confetti depigmentation following application of Leucodinine B on a chloasma].
=============================================================
Ann Dermatol Venereol 1982;109(10):899-900
Colomb D
Publication Types:
Letter
=============================================================
=============================================================
48.) Ruby laser treatment of melasma and postinflammatory hyperpigmentation.
=============================================================
Dermatol Surg 1995 Nov;21(11):994
Kopera D, Hohenleutner U
Publication Types:
Comment
Letter
Comment on
J Dermatol Surg Oncol. 1994 Sep;20(9):592-7
=============================================================
49.) The bleaching Treatments
=============================================================
source: DERMATOLOGIC FORUM
DR. M. linares Barrios. Spain.
Fórmula depigmentante de Klingman: Hidroquinona al 2-5%, ácido retinoico al 0.025, valerato de betametasona al 0.1% en crema de base Beeler. c.s.p. 60 grs Envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Hidroquinona al 2-5%, ácido retinoico al 0.025, indometacina al 3-5% en crema de base Beeler. c.s.p. 60 grs Envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Hidroquinona al 4%, ácido retinoico al 0.01, triamcinolona al 0.1% en excipiente O/W c.s.p. 60 grs. Envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Crema de base Beeler con hidroquinona: Alcohol cetílico 15, cera blanca 1, propilenglicol 10, laurilsulfato sódico 2, hidroquinona base 4, ácido retinoico 0.05, acetónido de triamcinolona 0.05, agua destilada c.s.p 100 m.s.a. Envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Acido Kojico al 4%, ácido retinoico al 0.05 en excipiente O/W. c.s.p. 60 grs envasar en tubo metálico . Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Acido Kojico al 2%, ácido glicólico al 5% en excipiente O/W. c.s.p. 60 grs envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Hidroquinona al 2%, ácido glicólico al 10% en excipiente O/W. c.s.p. 60 grs envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Hidroquinona al 2%, ácido kójico al 2% valerato de betametasona al 0.1% en crema de base Beeler c.s.p. 60 grs envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Hidroquinona al 2-5%, ácido kójico al 3% aceite de rosa de mosqueta al 5-10% antioxidante c.s en crema de base Beeler c.s.p. 60 grs envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Hidroquinona al 5%, ácido retinoico al 0.1, hidrocortisona al 1% en crema de base Beeler. c.s.p. 60 grs envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Hidroquinona al 4%, ácido retinoico al 0.1, ácido láctico al 7% en hidrogel c.s.p. 60 grs envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
Acido azelaico al 20%, ácido retinoico al 0.05 en crema de base Beeler. c.s.p. 60 grs envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE.
Acido ascórbico al 2-5%, antioxidante c.s, en crema de base Beeler. c.s.p. 60 grs envasar en tubo metálico. Proteger de la luz. Aplicar por la noche en las manchas. No debe de extrañarse si se irrita en las primeras aplicaciones. Esto es normal. Lavar bien la cara al día siguiente empleando crema de protección solar SIEMPRE
BIBLIOGRAFIA
------------
1.- Bolognia JL, Sodi SA, Osber MP et al: Enhancement of the depigmenting effect of hydroquinone by cistamine and buthonine sulfoximine Br J Dermatol 1995;133:349-57
2.- Funasaka Y, Komoto M, Ichihashi M Depigmenting effect of alpha-tocopheryl ferulate on normal human melanocytes.Pigment Cell Res 2000;13 Suppl 8:170-4
3.- Funasaka Y, Chakraborty AK, Komoto M, Ohashi A, Ichihashi M The depigmenting effect of alpha-tocopheryl ferulate on human melanoma cells. Br J Dermatol 1999 Jul;141(1):20-9
4.- Maeda K, Fukuda M Arbutin: mechanism of its depigmenting action in human melanocyte culture. J Pharmacol Exp Ther 1996 Feb;276(2):765-9
5.- Napolitano A, d'Ischia M, Prota G, Havens M, Tramposch K 2-Aryl-1,3-thiazolidines as masked sulfhydryl agents for inhibition of melanogenesis.Biochim Biophys Acta 1991 Mar 4;1073(2):416-22
6.- Fleischer AB Jr, Schwartzel EH, Colby SI, Altman DJ. The combination of 2% 4-hydroxyanisole (Mequinol) and 0.01% tretinoin is effective in improving the appearance of solar lentigines and related hyperpigmented lesions in two double-blind multicenter clinical studies. J Am Acad Dermatol 2000 Mar;42(3):459-67
7.- Nakajima M, Shinoda I, Mikogami T, Iwamoto H, Hashimoto S, Miyauchi H, Fukuwatari Y, Hayasawa H Beta-lactoglobulin suppresses melanogenesis in cultured human melanocytes.Pigment Cell Res 1997 Dec;10(6):410-3
8.- Nakajima M, Shinoda I, Samejima Y, Miyauchi H, Fukuwatari Y, Hayasawa H Kappa-casein suppresses melanogenesis in cultured pigment cells. Pigment Cell Res 1996 Oct;9(5):235-9
9.- Jimbow M, Marusyk H, Jimbow K. The in vivo melanocytotoxicity and depigmenting potency of N-2,4-acetoxyphenyl thioethyl acetamide in the skin and hair. Br J Dermatol 1995 Oct;133(4):526-36
10.- Tandon M, Thomas PD, Shokravi M, Singh S, Samra S, Chang D, Jimbow K Synthesis and antitumour effect of the melanogenesis-based antimelanoma agent N-propionyl-4-S-cysteaminylphenol.Biochem Pharmacol 1998 Jun 15;55(12):2023-9
11.- Jimbow K N-acetyl-4-S-cysteaminylphenol as a new type of depigmenting agent for the melanoderma of patients with melasma. Arch Dermatol 1991 Oct;127(10):1528-34
12.- Curso de formulación magistral. Barcelona, Enero 2000. Dres Umbert y Llambí
==================================================================
DATA-MEDICOS/DERMAGIC-EXPRESS No 3-(97) 27/02/2.001 DR. JOSE
LAPENTA R.
===================================================================
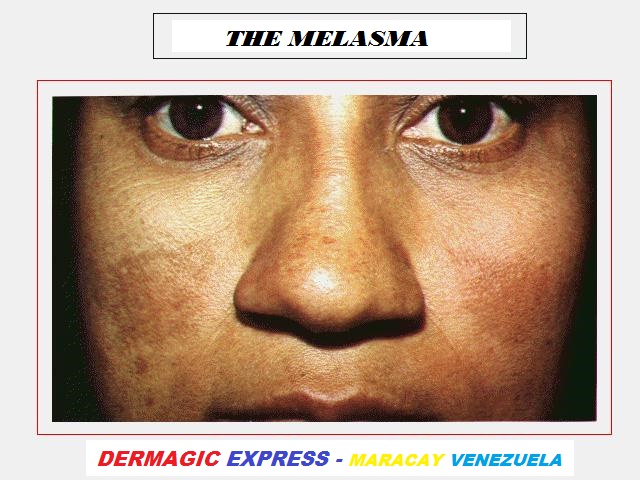
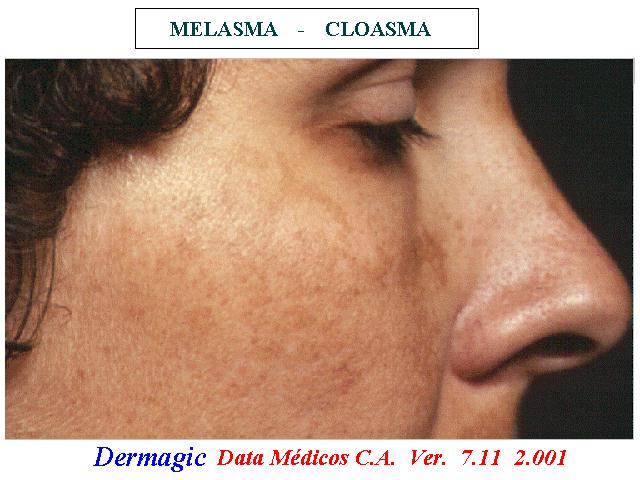
|

