| The Smallpox II,
the return of a battle that we never win./ Chapter II La Viruela II, el regreso de una batalla que nunca ganamos
/ Capitulo II
Data-Medicos
Dermagic/Express No. 3-(101)
30 Junio 2.001.30 June 2.001.
============================================================
REFERENCIAS BIBLIOGRAFICAS / BIBLIOGRAPHICAL REFERENCES
============================================================
=============================================================
41.) [Circulation of virus and interspecies contamination in wild animals].
42.) [Eradication of smallpox, already 20 years ago].
43.) 'Bacilli and bullets': William Osler and the antivaccination movement.
44.) A pediatrician's view. Skin manifestations of bioterrorism.
45.)Accidental exposure to smallpox vaccine, Russian Federation.
46.) [Antiviral vaccines].
47.) [Biohazards due to Orthopoxvirus: should we re-vaccinate against smallpox]?
48.) Long-term protective immunity to rinderpest in cattle following a single vaccination with a recombinant vaccinia virus expressing the virus haemagglutinin protein.
49.) Adverse reactions to smallpox vaccine: the Israel Defense Force experience, 1991 to 1996. A comparison with previous surveys.
50.) Smallpox: a possible public health threat, again.
51.) Graves' disease presenting as localized myxoedematous infiltration in a smallpox vaccination scar.
52.) ["Biological weapons"--the return of epidemics]?
53.) Adventures with poxviruses of vertebrates.
54.) The cost of disease eradication. Smallpox and bovine tuberculosis.
55.) The threat of biological terrorism: a public health and infection control reality.
56.) Alastrim smallpox variola minor virus genome DNA sequences.
57.) The role of the clinical laboratory in managing chemical or biological terrorism.
58.) Cidofovir protects mice against lethal aerosol or intranasal cowpox virus challenge.
59.) The threat of bioterrorism: a reason to learn more about anthrax and smallpox.
60.) Demographic impact of vaccination: a review.
61.) Lessons from the eradication campaigns.
62.) [Smallpox dilemma].
63.) Paramunity-inducing effects of vaccinia strain MVA.
64.) [Historical review of smallpox, the eradication of smallpox and the attenuated smallpox MVA vaccine].
65.)Current Status of Smallpox Vaccine
66.) Production of recombinant subunit vaccines: protein immunogens, live delivery systems and nucleic acid vaccines.
67.) Natural history and pathogenesis as they affect clinical trials.
68.) BERNA: a century of immunobiological innovation.
69.) Immune modulation by proteins secreted from cells infected by vaccinia virus.
70.) Smallpox: Clinical and Epidemiologic Features
71.) Nature, nurture and my experience with smallpox eradication.
72.) Vaccines in civilian defense against bioterrorism.
73.) Smallpox eradication. Destruction of variola virus stocks.
74.) [Attempts to inoculate against plague in the eighteenth and nineteenth centuries].
75.) Adventures with poxviruses of vertebrates.
76.) Smallpox as a biological weapon: medical and public health management. Working Group on Civilian Biodefense.
77.) A variant of variola virus, characterized by changes in polypeptide and endonuclease profiles.
78.) Eradication of vaccine-preventable diseases.
79.) President revokes plan to destroy smallpox.
80.) Re-emergence of monkeypox in Africa: a review of the past six years.
81.) Scientists split on US smallpox decision.
82.) Smallpox preservation advisable.
83.) The major epidemic infections: a gift from the Old World to the New?
84.) New technologies for vaccines.
85.) Aftermath of a hypothetical smallpox disaster.
86.) Strengthening National Preparedness for Smallpox: an Update
87.) Smallpox: An attack scenario.
=============================================================
=============================================================
41.) [Circulation of virus and interspecies contamination in wild animals].
=============================================================
Bull Soc Pathol Exot 2000 Jul;93(3):156 Related Articles, Books, LinkOut
[Article in French]
Osterhaus A.
Universite de Rotterdam, Pays-Bas.
Paradoxically, just when we have succeeded in eradicating and/or bringing under control the major viral infections (smallpox, poliomyelitis, measles) numerous viral infections are emerging in man and in animals. Changes in our social environment, technological and ecological equilibrium have facilitated this phenomenon. Furthermore, certain of these viruses have demonstrated an almost unlimited capacity to adapt genetically to environmental change. HIV has already infected 40 million individuals, but monkeypox, Ebola, simian herpes can cause epidemics with serious if not fatal outcomes. Haemorrhagic fever epidemics have resulted from human contact with Flavivirus infected rodents and insects. Paramyxoviruses and morbiliviruses can cause fatal outcomes in man and animals. And the three influenza epidemics having occurred in the 20th century all came from the type A avian reservoir. The often complex combinations of predisposing factors having facilitated the emergence of several epidemics merit further consideration.
=============================================================
42.) [Eradication of smallpox, already 20 years ago].
=============================================================
Bull Acad Natl Med 2000;184(1):89-99; discussion 99-104
[Article in French]
Bazin H.
University of Louvain, Faculty of medicine, Experimental Immunology Unit, Paris.
Smallpox, an infectious disease that has killed and maimed hundreds of thousands of people through the ages and across all continents, has disappeared. Its eradication has been the result of an enormous and intense collective effort carried out over several years. Furthermore, it made possible the elimination of many of the risks associated with vaccination against smallpox, which had rare but very real side effects. The 20th anniversary of this momentous event will take place on 8th May 2000.
=============================================================
43.) 'Bacilli and bullets': William Osler and the antivaccination movement.
=============================================================
South Med J 2000 Aug;93(8):763-7
Greenberg SB.
Department of Medicine, Microbiology and Immunology, Baylor College of Medicine, Houston, Texas 77030, USA.
Public discourse concerning current vaccination recommendations has dramatically increased. The current battle is not new, having had a lengthy foreshadowing during the 19th and early 20th centuries. Over a 30-year period, a concerted effort to limit the use of smallpox vaccine grew at the very time typhoid vaccines were being developed and advocated for widespread prevention. As a long time advocate for widespread smallpox vaccination and a supporter of the newly tested typhoid vaccine, Sir William Osler entered the public debate at the beginning of World War I. Osler was asked to address the officers and men in the British army on the need for typhoid vaccination. His speech entitled "Bacilli and Bullets" outlined the medical reasons for getting inoculated against typhoid. Osler's strong support for typhoid vaccination of the British troops was met by opposition in Parliament but not by most of the troops. Osler's arguments in support of vaccination failed to respond to the concept of "conscientious objection," which was central to the antivaccinationists' argument. Similar arguments are being propounded by current antivaccination groups.
=============================================================
44.) A pediatrician's view. Skin manifestations of bioterrorism.
=============================================================
Pediatr Ann 2000 Jan;29(1):7-9
Cross JT Jr, Altemeier WA 3rd.
The physician must be in contact with the local public health infrastructure as soon as a potential biological agent is perceived as possible. Most states are now setting up contingency plans and means to address these issues in a systematic way. This involves using local health departments, police departments, fire departments, National Guard units, and federal agencies such as the CDC and the FBI. The key component, however, is actually identifying a biological agent in the community and then moving quickly to isolate those who may be at risk of spreading the infection.
=============================================================
45.)Accidental exposure to smallpox vaccine, Russian Federation.
=============================================================
Wkly Epidemiol Rec 2000 Jun 23;75(25):202
=============================================================
=============================================================
46.) [Antiviral vaccines].
=============================================================
Med Trop (Mars) 1999;59(4 Pt 2):522-6 Related Articles, Books
[Article in French]
Girard M.
Centre Europeen de Recherche en Immunologie et Virologie, Lyon, France. [email protected]
Vaccination has been successful in controlling numerous diseases in man and animals. Smallpox has been eradicated and poliomyelitis is on the verge of being eradicated. The traditional immunization arsenal includes vaccines using live, attenuated, and inactivated organisms. DNA recombinant technology has added two new types of vaccines, i.e. subunit vaccines based on purified antigens produced by genetic engineering in bacterial, yeast, or animal-cell cultures and live recombinant vaccines based on attenuated bacterial or viral vectors. Currently the best known examples of these new vaccines are those using poxvirus vectors (vaccinia virus, canarypox virus, or fowlpox virus) but new vectors are under development. Another application for genetic engineering in the field of vaccinology is the development of DNA vaccines using naked plasmid DNA. This technique has achieved remarkable results in small rodents but its efficacy, safety, and feasibility in man has yet to be demonstrated. Numerous studies are now under way to improve the process. In the field of synthetic vaccines, lipopeptides have shown promise for induction of cell immune response. Development of vaccines for administration by the oral or nasal route may one day revolutionize vaccination techniques. However, effective vaccines against hepatitis C and HIV have stalled in the face of the complexity and pathophysiology of these diseases. These are the greatest challenges confronting scientists at the dawn of the new millennium.
=============================================================
47.) [Biohazards due to Orthopoxvirus: should we re-vaccinate against smallpox]?
=============================================================
Med Trop (Mars) 1999;59(4 Pt 2):483-7
[Article in French]
Georges AJ, Georges-Courbot MC.
Centre International de Recherche Medicale de Franceville, Gabon. [email protected]
Although the WHO declared global smallpox eradication in 1980, the Orthopoxvirus remains a source of concern for several reasons. Firstly, stocks of the smallpox virus have been preserved for experimental use (at least officially in the USA and Russia) so that an escaped isolate could lead to reemergence and spread of the disease worldwide. Secondly discontinuation of smallpox vaccination programs has led to dwindling acquired immunity in the world population thus raising the risk of epidemic extension of several Orthopoxvirus zoonoses (e.g., monkeypox). Thirdly stocks of camelpox virus which is very similar to Smallpox virus and was intended for biological warfare were discovered during the Gulf War in 1991 and pose a potentially serious threat. Finally official stocks of Smallpox virus could be stolen and used by bioterrorists. Thus reemergence of Orthopoxvirus including smallpox, monkeypox, cowpox, and camelpox is a real danger and contingency planning is needed to define prophylactic and therapeutic strategies to prevent and/or stop an epidemics. Adverse effects from earlier smallpox vaccine (vaccinia) in healthy people or immunocompromised people (congenital or acquired as in HIV infected patients) are absolute contraindications to smallpox vaccination at this time. Further research is needed to develop new vaccines (e.g., attenuated isolates of vaccinia) and effective treatment. This is the only valid reasons for postponing planned destruction of remaining Smallpox virus stocks.
=============================================================
48.) Long-term protective immunity to rinderpest in cattle following a single vaccination with a recombinant vaccinia virus expressing the virus haemagglutinin protein.
=============================================================
J Gen Virol 2000 Jun;81 Pt 6:1439-46
Ohishi K, Inui K, Barrett T, Yamanouchi K.
Institute for Animal Health, Pirbright Laboratory, Woking, Surrey GU24 0NF, UK.
A recombinant vaccine, produced by using a highly attenuated smallpox vaccine (LC16mO) as a vector and which expresses the rinderpest virus (RPV) haemagglutinin protein, has been developed. The properties of this vaccine, including its heat stability, efficacy in short-term trials, safety and genetic stability, have been confirmed in an earlier report. In the present study, the duration of the protective immunity generated by the vaccine in cattle was examined for up to 3 years following the administration of a single vaccination dose of 10(8) p.f.u. The vaccinated cattle were kept for 2 (group I) or 3 years (group II) and then challenged with a highly virulent strain of RPV. Four of five vaccinated cattle in group I and all six cattle in group II survived the challenge, some showing solid immunity without any clinical signs of rinderpest. Neutralizing antibodies were maintained at a significant level for up to 3 years and they increased rapidly following challenge. Lymphocyte proliferative responses to RPV were examined in group II cattle and were observed in four of the six vaccinated cattle in this group. The long-lasting protective immunity, in addition to the other properties confirmed previously, indicate the practical usefulness of this vaccine for field use.
=============================================================
49.) Adverse reactions to smallpox vaccine: the Israel Defense Force experience, 1991 to 1996. A comparison with previous surveys.
=============================================================
Mil Med 2000 Apr;165(4):287-9 Related Articles, Books
Haim M, Gdalevich M, Mimouni D, Ashkenazi I, Shemer J.
Army Health Branch, Medical Corps, Israel Defense Force, Israel.
The aim of the present study was to assess the post-smallpox vaccination complication rate in a cohort of Israel Defense Force recruits enlisted in the calendar years 1991 to 1996 and to compare it with rates reported, in similar age groups, in large surveys during the 1960s. The overall complication rate was 0.4 per 10,000 vaccinees, and the rate of severe complications was very low, similar to previously published data. We conclude that among young healthy adults, vaccination with smallpox vaccine is relatively safe and is associated with a low rate of complications. Severe complications were very rare in this age group in our study. However, the complication rate is increasing with the increased percentage of primary vaccinees.
=============================================================
50.) Smallpox: a possible public health threat, again.
=============================================================
Mo Med 2000 Apr;97(4):125
Thomas JR.
Publication Types:
Editorial
=============================================================
=============================================================
51.) Graves' disease presenting as localized myxoedematous infiltration in a smallpox vaccination scar.
=============================================================
Clin Exp Dermatol 2000 Mar;25(2):132-4
Pujol RM, Monmany J, Bague S, Alomar A.
Department of Dermatology, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain. [email protected]
We describe a 54-year-old woman with diffuse myxoedematous infiltration at the site of a smallpox vaccination scar as the presenting symptom of Graves' disease. Associated features included acute ocular symptoms (vascular congestion of the sclera, epiphora and blurred vision) and transient erythema on both shins. However, there were no signs of pretibial myxoedema. A number of neoplastic, inflammatory and systemic diseases may localize to scar tissue in skin, including at smallpox vaccination sites, but this case demonstrates the unusual occurrence of myxoedematous infiltration at such a site and illustrates a most atypical cutaneous presentation of Graves'disease.
=============================================================
52.) ["Biological weapons"--the return of epidemics]?
=============================================================
Pneumologie 2000 Feb;54(2):97-8 Related Articles, Books
[Article in German]
Fuchs HS.
=============================================================
=============================================================
53.) Adventures with poxviruses of vertebrates.
=============================================================
FEMS Microbiol Rev 2000 Apr;24(2):123-33
Fenner F.
John Curtin School of Medical Research, Australian National University, G.P.O. Box 334, Canberra, Australia. [email protected]
Because they were the largest of all viruses and could be visualised with a light microscope, the poxviruses were the first viruses to be intensively studied in the laboratory. It was clear from an early date that they caused important diseases of humans and their domestic animals, such as smallpox, cowpox, camelpox, sheeppox, fowlpox and goatpox. This essay recounts some of the early history of their recognition and classification and then expands on aspects of research on poxviruses in which the author has been involved. Studies on the best-known genus, Orthopoxvirus, relate to the use of infectious ectromelia of mice as a model for smallpox, embracing both experimental epidemiology and pathogenesis, studies on the genetics of vaccinia virus and the problem of non-genetic reactivation (previously termed 'transformation') and the campaign for the global eradication of smallpox. The other group of poxviruses described here, the genus Leporipoxvirus, came to prominence when the myxoma virus was used for the biological control of Australian wild rabbits. This provided a unique natural experiment on the coevolution of a virus and its host. Future research will include further studies of the many immunomodulatory genes found in all poxviruses of vertebrates, since these provide clues about the workings of the immune system and how viruses have evolved to evade it. Some of the many recombinant poxvirus constructs currently being studied may come into use as vaccines or for immunocontraception. A field that warrants study but will probably remain neglected is the natural history of skunkpox, raccoonpox, taterapox, yabapox, tanapox and other little-known poxviruses. A dismal prospect is the possible use of smallpox virus for bioterrorism.
=============================================================
54.) The cost of disease eradication. Smallpox and bovine tuberculosis.
=============================================================
Ann N Y Acad Sci 1999;894:83-91 Related Articles, Books
Nelson AM.
Department of Infectious and Parasitic Disease Pathology, Armed Forces Institute of Pathology, Washington, D.C. 20306-6000, USA. [email protected]
Although eradication is the ideal approach to reduce the economic and human health costs of disease, there may be both short- and long-term consequences. A $300 million effort succeeded in completely eradicating smallpox in less than ten years. The campaign was effective because variola virus produced acute illness, had no carrier stage or non-human reservoirs, and had an effective vaccine that was used in combination with international surveillance and public education. Bovine tuberculosis was completely eradicated in many U.S. herds at a cost of $450 million over 50 years using a "test and slaughter" program combined with meat inspection. Mycobacterium bovis often does not produce acute disease, persists in the carrier stage, has multiple non-human reservoirs, and easily crosses species. No effective vaccine or centralized global surveillance or eradication programs currently exist. Control measures result in significant economic losses. Smallpox eradication had limited economic consequences but has left much of world's population highly susceptible to zoonotic orthopoxviruses and to the use of smallpox as a biologic weapon. The primary threat of M. bovis exists in wildlife that share watering holes or pasture land with domestic stock. In the developed world, surveillance can minimize risks, but one-third of the world's population lacks effective agricultural and food safety programs, leaving them at substantial risk for zoonotic infection by M. bovis.
=============================================================
55.) The threat of biological terrorism: a public health and infection control reality.
=============================================================
Infect Control Hosp Epidemiol 2000 Jan;21(1):53-6
Leggiadro RJ.
Department of Pediatrics, Sisters of Charity Medical Center, Staten Island, New York 10310, USA.
Bioterrorism is an emerging public health and infection control threat. Potential biological agents include smallpox, anthrax, plague, tularemia, botulinum toxin, brucellosis, Q fever, viral encephalitis, hemorrhagic fever, and staphylococcal enterotoxin B. An understanding of the epidemiology, clinical manifestations, and management of the more likely candidate agents is critical to limiting morbidity and mortality from a biological event. Effective response requires an increased index of suspicion for unusual diseases or syndromes, with prompt reporting to health authorities to facilitate recognition of an outbreak and subsequent intervention. Hospital epidemiology programs will play a crucial role in this effort.
=============================================================
56.) Alastrim smallpox variola minor virus genome DNA sequences.
=============================================================
Virology 2000 Jan 20;266(2):361-86
Shchelkunov SN, Totmenin AV, Loparev VN, Safronov PF, Gutorov VV, Chizhikov VE, Knight JC, Parsons JM, Massung RF, Esposito JJ.
Department of Molecular Biology of Genomes, State Research Center of Virology and Biotechnology (Vector), Koltsovo, Novosibirsk Region, 633159, Russia. [email protected]
Alastrim variola minor virus, which causes mild smallpox, was first recognized in Florida and South America in the late 19th century. Genome linear double-stranded DNA sequences (186,986 bp) of the alastrim virus Garcia-1966, a laboratory reference strain from an outbreak associated with 0.8% case fatalities in Brazil in 1966, were determined except for a 530-bp fragment of hairpin-loop sequences at each terminus. The DNA sequences (EMBL Accession No. Y16780) showed 206 potential open reading frames for proteins containing >/=60 amino acids. The amino acid sequences of the putative proteins were compared with those reported for vaccinia virus strain Copenhagen and the Asian variola major strains India-1967 and Bangladesh-1975. About one-third of the alastrim viral proteins were 100% identical to correlates in the variola major strains and the remainder were >/=95% identical. Compared with variola major virus DNA, alastrim virus DNA has additional segments of 898 and 627 bp, respectively, within the left and right terminal regions. The former segment aligns well with sequences in other orthopoxviruses, particularly cowpox and vaccinia viruses, and the latter is apparently alastrim-specific. Copyright 2000 Academic Press.
=============================================================
57.) The role of the clinical laboratory in managing chemical or biological terrorism.
=============================================================
Clin Chem 2000 Dec;46(12):1883-93
Jortani SA, Snyder JW, Valdes R Jr.
Departments of Pathology and Laboratory Medicine, University of Louisville School of Medicine, Louisville, KY 40292, USA.
BACKGROUND: Domestic and international acts of terrorism using chemicals and pathogens as weapons have recently attracted much attention because of several hoaxes and real incidents. Clinical laboratories, especially those affiliated with major trauma centers, should be prepared to respond rapidly by providing diagnostic tests for the detection and identification of specific agents, so that specific therapy and victim management can be initiated in a timely manner. As first-line responders, clinical laboratory personnel should become familiar with the various chemical or biological agents and be active participants in their local defense programs. APPROACH: We review the selected agents previously considered or used in chemical and biological warfare, outline their poisonous and pathogenic effects, describe techniques used in their identification, address some of the logistical and technical difficulties in maintaining such tests in clinical laboratories, and comment on some of the analytical issues, such as specimen handling and personal protective equipment. CONTENT: The chemical agents discussed include nerve, blistering, and pulmonary agents and cyanides. Biological agents, including anthrax and smallpox, are also discussed as examples for organisms with potential use in bioterrorism. Available therapies for each agent are outlined to assist clinical laboratory personnel in making intelligent decisions regarding implementation of diagnostic tests as a part of a comprehensive defense program. SUMMARY: As the civilian medical community prepares for biological and chemical terrorist attacks, improvement in the capabilities of clinical laboratories is essential in supporting counterterrorism programs designed to respond to such attacks. Accurate assessment of resources in clinical laboratories is important because it will provide local authorities with an alternative resource for immediate diagnostic analysis. It is, therefore, recommended that clinical laboratories identify their current resources and the extent of support they can provide, and inform the authorities of their state of readiness.
=============================================================
58.) Cidofovir protects mice against lethal aerosol or intranasal cowpox virus challenge.
=============================================================
J Infect Dis 2000 Jan;181(1):10-9
Bray M, Martinez M, Smee DF, Kefauver D, Thompson E, Huggins JW.
Virology Division, USAMRIID, Fort Detrick, MD 21702-5011, USA. [email protected]
The efficacy of cidofovir for treatment of cowpox virus infection in BALB/c mice was investigated in an effort to evaluate new therapies for virulent orthopoxvirus infections of the respiratory tract in a small animal model. Exposure to 2(-5)x10(6) pfu of cowpox virus by aerosol or intranasally (inl) was lethal in 3- to 7-week-old animals. One inoculation of 100 mg/kg cidofovir on day 0, 2, or 4, with respect to aerosol infection, resulted in 90%-100% survival. Treatment on day 0 reduced peak pulmonary virus titers 10- to 100-fold, reduced the severity of viral pneumonitis, and prevented pulmonary hemorrhage. The same dose on day -6 to 2 protected 80%-100% of inl infected mice, whereas 1 inoculation on day -16 to -8 or day 3 to 6 was partially protective. Cidofovir delayed but did not prevent the death of inl infected mice with severe combined immunodeficiency. Treatment at the time of tail scarification with vaccinia virus did not block vaccination efficacy.
=============================================================
59.) The threat of bioterrorism: a reason to learn more about anthrax and smallpox.
=============================================================
Cleve Clin J Med 1999 Nov-Dec;66(10):592-5, 599-600
Gordon SM.
Department of Infectious Disease, Cleveland Clinic USA.
Threats of domestic terrorism and international news about germ warfare research have forced us to recognize the potential menace of biological weapons. Both smallpox and anthrax could be used as biological weapons. It is important for physicians to reacquaint themselves with these diseases, because if a domestic attack were to occur, it might first be recognized when patients with unusual symptoms began presenting to hospitals and primary care physicians. In this article, we discuss symptoms and treatments for smallpox and anthrax, and suggest resources for physicians who wish to learn more about the subject.
=============================================================
60.) Demographic impact of vaccination: a review.
=============================================================
Vaccine 1999 Oct 29;17 Suppl 3:S120-5
Bonanni P.
Public Health and Epidemiology Department, University of Florence, Viale G.B. Morgagni 48, 50134, Florence, Italy. [email protected]
Vaccination is one of the most powerful means to save lives and to increase the level of health of mankind. However, the impact of immunization against the most threatening infectious agents on life expectancy has been the object of a still open debate. The main issues are: the relative influence of nutrition and infectious diseases on demographic patterns of populations; the possibility that lives saved thanks to vaccination are subsequently lost due to other competing causes of death; the positive indirect effect of immunization on other causes of death. With regard to past evidence, several data from the United Kingdom and Scandinavian countries show that the widespread use of smallpox vaccination starting at the beginning of the nineteenth century resulted in a marked and sustained decline not only of smallpox-related deaths, but also of the overall crude death rate, and contributed greatly to an unprecedented growth of European population.As to the present, it is estimated that 3 million children are saved annually by vaccination, but 2 million still die because they are not immunized. Tetanus, measles and pertussis are the main vaccine-preventable killers in the first years of life. Data from Bangladesh show that full implementation of EPI vaccines has the potential of reducing mortality by almost one half in children aged 1-4 years. Recent progress in the development of vaccines against agents responsible for much mortality in the developing countries make it possible to forecast a further substantial reduction of deaths for infectious diseases in the next century.
=============================================================
61.) Lessons from the eradication campaigns.
=============================================================
Vaccine 1999 Oct 29;17 Suppl 3:S53-5
Henderson DA.
The John Hopkins School of Hygiene and Public Health, Candler Building, Suite 850, 111 Market Place, Baltimore, MD 21202, USA.
Of seven global eradication programs this century, only two have relied primarily on vaccines for control measures - those against smallpox and poliomyelitis. Smallpox is history and polio could possibly achieve a similar status within the next decade. The hallmarks of these successful programs were surveillance and community outreach and involvement. However, a research agenda, so crucial to smallpox eradication, has largely been ignored or dismissed by polio program managers. This could prove to be a serious, even fatal error.
=============================================================
62.) [Smallpox dilemma].
=============================================================
Recenti Prog Med 1999 Sep;90(9):449-50
[Article in Italian]
Rossi G.
=============================================================
=============================================================
63.) Paramunity-inducing effects of vaccinia strain MVA.
=============================================================
Berl Munch Tierarztl Wochenschr 1999 Sep;112(9):329-33
Vilsmeier B.
Chair of Medical Microbiology, Infectious and Epidemic Diseases, Faculty of Veterinary Medicine, Ludwig-Maximilians-University of Munich.
Vaccinia virus MVA is harmless for humans and animals both locally and parenterally. It offers paraspecific activities similar to those of comparable attenuated viruses of other pox genera, e.g. avipox or parapox. At the systemic level, MVA protects baby mice against lethal challenge with vesicular stomatitis virus (dose-response curve). MVA raises phagocytosis and NK-cell activity in humans and animals, whilst encouraging the induction of interferon alpha, interleukin-2 and -12 and colony-stimulating activity at the same time. The paramunity-inducing properties of MVA make it an ideal vector for the insertion of foreign genes. It is superior to other virus vectors because of its complex function. Inactivated MVA is also suitable as an inducer of paramunity.
=============================================================
64.) [Historical review of smallpox, the eradication of smallpox and the attenuated smallpox MVA vaccine].
=============================================================
Berl Munch Tierarztl Wochenschr 1999 Sep;112(9):322-8
[Article in German]
Mayr A.
Lehrstuhl fur Mikrobiologie und Seuchenlehre, Tierarztliche Fakultat, Ludwig-Maximilians-Universitat Munchen.
After the WHO had declared smallpox to be eradicated in 1980, smallpox vaccination ceased to be carried out in humans all over the world. The cutaneous inoculations carried out with live vaccines based on the vaccinia virus from 1798 onwards protected both the global population and, indirectly, the animals living with humans against orthopox infections in general. A large percentage of humans and animals no longer enjoy this protection. Idiopathic orthopox in animals (reservoir possibly rats and mice) are thus experiencing a renaissance, posing a threat to humans and animals. The paper provides an historical retrospective of smallpox epidemics in humankind, their course of development and methods employed to combat this disease, commencing long before the birth of Christ with primitive attempts in China and India and from the end of the 18th century with increasingly enhanced methods, most recently with worldwide smallpox vaccination programmes using live vaccinia vaccines. Smallpox vaccination was always accompanied by a variety of complications, especially postvaccinal encephalitis. The MVA strain was developed to reduce or prevent such adverse effects. MVA has meanwhile proved its worth both as a parenteral vaccine against orthopox infections in humans and animals and as a vector for insertion of foreign genes. The history of smallpox, the fight against this disease and the development of MVA are documented with the help of figures and tables.
=============================================================
65.)Current Status of Smallpox Vaccine
=============================================================
James W. LeDuc and John Becher
Centers for Disease Control and Prevention, Atlanta, Georgia, USA Vol. 5, No. 4
July–August
Letters
To the Editor: The possible use of smallpox virus as a weapon by terrorists has stimulated growing international concern and led to a recent review by the World Health Organization of the global availability of smallpox vaccine. This review found approximately 60 million doses worldwide, with little current vaccine manufacture, although limited vaccine seed remains available (1). Ongoing discussions in the United States suggest that the national stockpile should contain at least 40 million doses to be held in reserve for emergency use, including in case of a terrorist release of smallpox virus (O'Toole, this issue, pp. 540-6).
The current U.S. stockpile contains approximately 15.4 million doses of vaccinia vaccine (Dryvax) made from the New York City Board of Health strain of vaccinia and was produced by Wyeth Laboratories in 13 separate lots. The vaccine is lyophylized in glass vials with rubber stoppers and sealed with a metal band. When rehydrated, each vial contains 100 doses and has a potency of at least 108 plaque-forming units (pfu)/ml. Some vials of the vaccine stockpile have shown elevated moisture levels and thus failed routine quality control testing; however, the vaccine in these vials remains potent, and the failed lots have not been discarded.
The diluent used to rehydrate the vaccine contains brilliant green, which makes the vaccine easier to visualize when administered with bifurcated needles. Over time, the brilliant green has deteriorated, and most of the available diluent does not pass quality control. Discussions are under way with Wyeth to begin production of sufficient new diluent for the entire stockpile.
The vaccine is administered by superficial inoculation (scarification) with a bifurcated needle. Fewer than 1 million bifurcated needles are held as part of the stockpile. As with the diluent, Wyeth has been requested to produce additional bifurcated needles.
Vaccinia virus produces adverse reactions in a small percentage of vaccinated persons. Adverse reactions are treated with vaccinia immune globulin (VIG), currently only available from Baxter Healthcare Corporation (5,400 vials of VIG in stock). Each vial contains 5 ml of VIG; the recommended dose for postvaccine complications is 0.6 ml per kg of body weight. This volume is sufficient to treat adverse reactions in approximately 675 adults. Further, the entire stockpile of VIG has been placed on hold while the cause of a slight pink discoloration is investigated. Until the cause of the discoloration is determined or another approved supply of VIG is obtained, no vaccinia vaccine is being released. While unknown, the rate of adverse reactions in today's population is likely to be greater than seen during the global eradication campaign because of recent increases in the number of immunocompromised persons. The Department of Defense has recently contracted the processing of new lots of VIG (to be administered intravenously rather than by the intramuscular route like existing VIG stocks); however, maintaining adequate stocks of VIG will remain a challenge.
In the event of release of smallpox virus, persons at high risk and persons exposed but not yet showing clinical illness would be vaccinated immediately. Intensive case detection and vaccination of contacts and other persons at risk would follow. All vaccine, including lots retained after failed quality control tests, would be made available for emergency use. Previous studies have found that more than 90% of susceptible persons respond to vaccinia virus with a titer of 107 pocks/ml (2). In an emergency, consideration would be given to diluting the existing vaccine as much as 10-fold, so that each vial could conceivably contain 1,000 doses of vaccine, rather than the current 100 doses. The present vaccine container is sufficiently large to accommodate the added diluent. The absence of sufficient quantities of VIG to protect against adverse reactions during a mass immunization campaign would necessitate careful screening of those receiving the vaccine; some persons with adverse reactions would likely go untreated.
While the intentional release of smallpox virus would represent a global emergency, the existing national stockpile could be effectively used to limit the spread of disease and buy time while the pharmaceutical industry begins emergency vaccine production.
James W. LeDuc and John Becher
Centers for Disease Control and Prevention, Atlanta, Georgia, USA
References
World Health Organization. Report of the meeting of the ad hoc committee on Orthopox virus infections. Department of Communicable Disease Surveillance and Response. WHO, 14-15 January 1999.
Cockburn WC, Cross RM, Downie AW, Dumbell KR, Kaplan C, Mclean D, et al. Laboratory and vaccination studies with dried smallpox vaccines. Bull World Health Organ 1957;16:63-77.
=============================================================
66.) Production of recombinant subunit vaccines: protein immunogens, live delivery systems and nucleic acid vaccines.
=============================================================
J Biotechnol 1999 Jul 30;73(1):1-33 Related Articles, Books
Liljeqvist S, Stahl S.
Department of Biotechnology, Royal Institute of Technology (KTH), Stockholm, Sweden.
The first scientific attempts to control an infectious disease can be attributed to Edward Jenner, who, in 1796 inoculated an 8-year-old boy with cowpox (vaccinia), giving the boy protection against subsequent challenge with virulent smallpox. Thanks to the successful development of vaccines, many major diseases, such as diphtheria, poliomyelitis and measles, are nowadays kept under control, and in the case of smallpox, the dream of eradication has been fulfilled. Yet, there is a growing need for improvements of existing vaccines in terms of increased efficacy and improved safety, besides the development of completely new vaccines. Better technological possibilities, combined with increased knowledge in related fields, such as immunology and molecular biology, allow for new vaccination strategies. Besides the classical whole-cell vaccines, consisting of killed or attenuated pathogens, new vaccines based on the subunit principle, have been developed, e.g. the Hepatitis B surface protein vaccine and the Haemophilus influenzae type b vaccine. Recombinant techniques are now dominating in the strive for an ideal vaccine, being safe and cheap, heat-stable and easy to administer, preferably single-dose, and capable of inducing broad immune response with life-long memory both in adults and in infants. This review will describe different recombinant approaches used in the development of novel subunit vaccines, including design and production of protein immunogens, the development of live delivery systems and the state-of-the-art for nucleic acids vaccines.
=============================================================
67.) Natural history and pathogenesis as they affect clinical trials.
=============================================================
Dev Biol Stand 1998;95:61-7
Moxon ER.
Institute of Molecular Medicine, University of Oxford Department of Paediatrics and Oxford Vaccine Group, John Radcliffe Hospital, UK.
Careful observations on the natural history of infectious diseases have been the inspiration behind many successful vaccines, including Jenner's successful demonstration of protection against smallpox. Many "experiments of nature" provide powerful data on the key components of protective immunity. An understanding of the basis of protective immunity in absolute terms or, more realistically, through the proxy of surrogates of immunity, lies at the heart of clinical trials of vaccines. An understanding of infectious disease pathogenesis is also critical in defining and distinguishing immunisation strategies that aim to prevent infection (e.g. measles vaccine) as distinct from prevention of disease (e.g. tetanus toxoid). Coupled to classical epidemiology and the careful analysis of clinical data, the tools of molecular and cell biology have revolutionised the tools available for vaccine research, including clinical trials. Molecular techniques have provided tools for investigating the population structure of pathogens. The importance of population diversity and its associated antigenic variation is a key factor in designing and carrying out clinical trials of vaccines.
=============================================================
68.) BERNA: a century of immunobiological innovation.
=============================================================
Vaccine 1999 Oct 1;17 Suppl 2:S1-5
Cryz SJ.
BERNA, Swiss Serum and Vaccine Institute Berne, Rehhagstrasse 79, CH-3018, Bern, Switzerland.
At the time the Swiss Serum and Vaccine Institute Berne (BERNA) was found in 1898, few vaccines or immune globulins were available. This short list included vaccines against cholera, typhoid fever, plague, smallpox and rabies and equine anti-tetanus and diphtheria immune globulins. Furthermore, their use was restricted due to limited production capacity, uncertainty regarding safety and no public health infrastructure to promote their utilization. Today, safe and effective vaccines exist for more than 30 infectious diseases while human hyperimmune globulins exist to treat or prevent rabies, tetanus, respiratory syncytial virus, cytomegalovirus, hepatitis A, hepatitis B, and herpes virus (Varicella zoster) infections. Throughout its 100 years of existence, BERNA has played a key role in the evolution of the field by introducing novel technology leading to safer, and more efficacious vaccines. It was a pioneer in the development of freeze dried smallpox vaccine free from bacterial contamination. The Salmonella typhi Ty21a typhoid fever vaccine strain demonstrated that oral immunization against enteric bacterial pathogens was not only feasible, but could be accomplished with a virtual lack of attendant adverse reactions. This finding has served as an impetus to develop other live attenuated bacterial strains not only as vaccines, but also as vectors for vaccine antigens and gene therapy. One such example is Vibrio cholerae CVD 103-HgR, the first live vaccine for human use derived through recombinant DNA technology. Subsequent studies have shown that these two vaccine strains can be combined without sacrificing safety or immunogenicity, setting the cornerstone for combined orally administered vaccines. Recently, a novel vaccine antigen delivery system, termed virosomes, has been utilized to construct hepatitis A and influenza vaccines. Such vaccines elicit fewer local adverse reactions than their classical counterparts and display enhanced immunogenicity. Virosome-formulated influenza vaccine has also been shown to be safe and immunogenic, when administered by the intranasal route.
=============================================================
69.) Immune modulation by proteins secreted from cells infected by vaccinia virus.
=============================================================
Arch Virol Suppl 1999;15:111-29
Smith GL, Symons JA, Alcami A.
Sir William Dunn School of Pathology, University of Oxford, U.K.
Vaccinia virus comprises the live vaccine that was used for vaccination against smallpox. Following the eradication of smallpox, vaccinia virus was developed as an expression vector that is now used widely in biological research and vaccine development. In recent years vaccinia virus and other poxviruses have been found to express a collection of proteins that block parts of the host response to infection. Some of these proteins are secreted from the infected cell where they bind and neutralise host cytokines, chemokines and interferons (IFN). In this paper three such proteins that bind interleukin (IL)-1 beta, type I IFNs and CC chemokines are described. The study of these immunomodulatory molecules is enhancing our understanding of virus pathogenesis, yielding fundamental information about the immune system, and providing new molecules that have potential application for the treatment of immunological disorders or infectious diseases.
=============================================================
70.) Smallpox: Clinical and Epidemiologic Features
=============================================================
D. A. Henderson
Johns Hopkins Center for Civilian Biodefense Studies, Baltimore, Maryland, USA
Clinical and Epidemiologic Characteristics of Smallpox
Smallpox is a viral disease unique to humans. To sustain itself, the virus must pass from person to person in a continuing chain of infection and is spread by inhalation of air droplets or aerosols. Twelve to 14 days after infection, the patient typically becomes febrile and has severe aching pains and prostration. Some 2 to 3 days later, a papular rash develops over the face and spreads to the extremities (Figure 1). The rash soon becomes vesicular and later, pustular (Figure 2). The patient remains febrile throughout the evolution of the rash and customarily experiences considerable pain as the pustules grow and expand. Gradually, scabs form, which eventually separate, leaving pitted scars. Death usually occurs during the second week.
Figure 1
Click to view enlarged image
Figure 1. Most cases of smallpox are clinically typical and readily able to be diagnosed. Lesions on each area of the body are at the same stage of development, are deeply embedded in the skin, and are more densely concentrated on the face and extremities.
The disease most commonly confused with smallpox is chickenpox, and during the first 2 to 3 days of rash, it may be all but impossible to distinguish between the two. However, all smallpox lesions develop at the same pace and, on any part of the body, appear identical. Chickenpox lesions are much more superficial and develop in crops. With chickenpox, scabs, vesicles, and pustules may be seen simultaneously on adjacent areas of skin. Moreover, the rash in chickenpox is more dense over the trunk (the reverse of smallpox), and chickenpox lesions are almost never found on the palms or soles.
In 5% to 10% of smallpox patients, more rapidly progressive, malignant disease develops, which is almost always fatal within 5 to 7 days. In such patients, the lesions are so densely confluent that the skin looks like crepe rubber; some patients exhibit bleeding into the skin and intestinal tract. Such cases are difficult to diagnose, but they are exceedingly infectious.
Smallpox spreads most readily during the cool, dry winter months but can be transmitted in any climate and in any part of the world. The only weapons against the disease are vaccination and patient isolation. Vaccination before exposure or within 2 to 3 days after exposure affords almost complete protection against disease. Vaccination as late as 4 to 5 days after exposure may protect against death. Because smallpox can only be transmitted from the time of the earliest appearance of rash, early detection of cases and prompt vaccination of all contacts is critical.
Smallpox Vaccination
Figure 2
Click to view enlarged image
Figure 2. The lesions of chickenpox develop as a series of "crops" over several days and are very superficial. Papules, vesicles, pustules, and scabs can be seen adjacent to each other. The trunk is usually more affected than the face or extremities.
Smallpox vaccination is associated with some risk for adverse reactions; the two most serious are postvaccinal encephalitis and progressive vaccinia. Postvaccinal encephalitis occurs at a rate of 3 per million primary vaccinees; 40% of the cases are fatal, and some patients are left with permanent neurologic damage. Progressive vaccinia occurs among those who are immunosuppressed because of a congenital defect, malignancy, radiation therapy, or AIDS. The vaccinia virus simply continues to grow, and unless these patients are treated with vaccinia immune globulin, they may not recover. Pustular material from the vaccination site may also be transferred to other parts of the body, sometimes with serious results.
Routine vaccination is only recommended for laboratory staff who may be exposed to one of the orthopoxviruses. There are two reasons for this. First is the risk for complications. Second, U.S. national vaccine stocks are sufficient to immunize only 6 to 7 million persons. This amount is only marginally sufficient for emergency needs. Plans are now being made to expand this reserve. However, at least 36 months are required before large quantities can be produced.
The potential of smallpox as a biological weapon is most dramatically illustrated by two European smallpox outbreaks in the 1970s. The first occurred in Meschede, Germany, in 1970 (1). This outbreak illustrates that smallpox virus in an aerosol suspension can spread widely and infect at very low doses.
Another outbreak occurred in Yugoslavia in February 1972 (1). Despite routine vaccination in Yugoslavia, the first case in the 1972 outbreak resulted in 11 others; those 11, on average, each infected 13 more. Other outbreaks in Europe from 1958 on showed that such explosive spread was not unusual during the seasonal period of high transmission, i.e., December through April. One can only speculate on the probable rapidity of spread of the smallpox virus in a population where no one younger than 25 years of age has ever been vaccinated and older persons have little remaining residual immunity.
Where might the virus come from? At one time, it was believed that the smallpox virus was restricted to only two high-security laboratories, one at the Centers for Disease Control and Prevention in Atlanta, Georgia, and one at the Russian State Centre for Research on Virology and Biotechnology, Koltsovo, Novosibirsk Region. By resolution of the 1996 World Health Assembly (WHA), those stocks were slated to be destroyed at the end of June 1999. The desirability of such an action was reaffirmed by a World Health Organization Expert Committee in January 1999. On May 22, 1999, WHA, however, passed a resolution postponing destruction until 2002, by which time any promise of the variola virus stocks for public health research could be determined. Destruction of the virus would be at least one step to limit the risk for the reemergence of smallpox. However, despite widespread acceptance of the 1972 Bioweapons Convention Treaty, which called for all countries to destroy their stocks of bioweapons and to cease all research on offensive weapons, other laboratories in Russia and perhaps in other countries maintain the virus. Iraq and the Soviet Union were signatories to the convention, as was the United States. However, as reported by the former deputy director of the Russian Bioweapons Program, officials of the former Soviet Union took notice of the world's decision in 1980 to cease smallpox vaccination, and in the atmosphere of the cold war, they embarked on an ambitious plan to produce smallpox virus in large quantities and use it as a weapon. At least two other laboratories in the former Soviet Union are now reported to maintain smallpox virus, and one may have the capacity to produce the virus in tons at least monthly. Moreover, Russian biologists, like physicists and chemists, may have left Russia to sell their services to rogue governments.
Smallpox is rated among the most dangerous of all potential biological weapons, with far-reaching ramifications.
Dr. Henderson is a distinguished service professor at the Johns Hopkins University, holding an appointment in the Department of Epidemiology. Dr. Henderson directed the World Health Organization's global smallpox eradication campaign (1966-1977) and helped initiate WHO's global program of immunization in 1974. He also served as deputy assistant secretary and senior science advisor in the Department of Health and Human Services.
Address for correspondence: D. A. Henderson, Johns Hopkins Center for Civilian Biodefense Studies, 111 Market Place, Ste. 850, Baltimore, MD 21202, USA; fax: 410-223-1665; e-mail: [email protected].
Reference
1. Henderson DA. Bioterrorism as a public health threat. Emerg Infect Dis 1998;4:488-92.
=============================================================
71.) Nature, nurture and my experience with smallpox eradication.
Med J Aust 1999 Dec 6-20;171(11-12):638-41
=============================================================
Fenner F.
John Curtin School of Medical Research, Australian National University, Canberra, ACT. [email protected]
Publication Types:
Biography
Historical article
=============================================================
=============================================================
72.) Vaccines in civilian defense against bioterrorism.
=============================================================
Emerg Infect Dis 1999 Jul-Aug;5(4):531-3
Russell PK.
Johns Hopkins School of Public Health, Baltimore, MD, USA. [email protected]
=============================================================
=============================================================
73.) Smallpox eradication. Destruction of variola virus stocks.
=============================================================
Wkly Epidemiol Rec 1999 Jun 18;74(24):188-91
=============================================================
=============================================================
74.) [Attempts to inoculate against plague in the eighteenth and nineteenth centuries].
=============================================================
Verh K Acad Geneeskd Belg 1999;61(2):385-409
[Article in Dutch]
Huygelen C.
In the middle of the 18th century, inoculation against smallpox became more and more common, and attempts were also made to test the same principle, viz. inoculation with the agents causing the disease for other human and animal diseases. It was tried for rinderpest, measles and sheep pox. In addition, there were some suggestions for using the principle against the plague. The disease had disappeared from Western Europe by this time, but still raged in eastern countries, such as Russia. However, the government rejected the proposal for trial inoculations in Moscow. During the first half of the 19th century, the plague was still widespread in the Middle East, where different European doctors worked on combatting it. The first documented inoculation trial was carried out by a certain Mr. Whyte, an English physician who inoculated himself and four assistants in 1801. All five died a few days later. In the following years, more tests were carried out, inter alia: in 1802, by Desgenettes, the chief physician of the French army in the Middle East; in 1803, by Eusebio Valli, an Italian physician in Constantinople; in 1818 and 1819 by Sola, a Spanish physician in Tangier. However, none of these tests produced clear results. During the epidemic in Egypt in the 1830s, further inoculation tests were carried out by a group of French plague specialists with the main aim of establishing whether the plague could be transmitted between humans. These tests did not result in any clear conclusions either. Following the discovery of the plague bacillus at the end of the 19th century, a number of different live and dead vaccines were developed, and were also used in endemic areas, but the level of efficiency has never become very clear. This is not really surprising, as even the disease itself often does not provide strong immunity, and reinfections are by no means uncommon.
=============================================================
75.) Adventures with poxviruses of vertebrates.
=============================================================
FEMS Microbiol Rev 2000 Apr;24(2):123-33
Fenner F.
John Curtin School of Medical Research, Australian National University, G.P.O. Box 334, Canberra, Australia. [email protected]
Because they were the largest of all viruses and could be visualised with a light microscope, the poxviruses were the first viruses to be intensively studied in the laboratory. It was clear from an early date that they caused important diseases of humans and their domestic animals, such as smallpox, cowpox, camelpox, sheeppox, fowlpox and goatpox. This essay recounts some of the early history of their recognition and classification and then expands on aspects of research on poxviruses in which the author has been involved. Studies on the best-known genus, Orthopoxvirus, relate to the use of infectious ectromelia of mice as a model for smallpox, embracing both experimental epidemiology and pathogenesis, studies on the genetics of vaccinia virus and the problem of non-genetic reactivation (previously termed 'transformation') and the campaign for the global eradication of smallpox. The other group of poxviruses described here, the genus Leporipoxvirus, came to prominence when the myxoma virus was used for the biological control of Australian wild rabbits. This provided a unique natural experiment on the coevolution of a virus and its host. Future research will include further studies of the many immunomodulatory genes found in all poxviruses of vertebrates, since these provide clues about the workings of the immune system and how viruses have evolved to evade it. Some of the many recombinant poxvirus constructs currently being studied may come into use as vaccines or for immunocontraception. A field that warrants study but will probably remain neglected is the natural history of skunkpox, raccoonpox, taterapox, yabapox, tanapox and other little-known poxviruses. A dismal prospect is the possible use of smallpox virus for bioterrorism.
=============================================================
76.) Smallpox as a biological weapon: medical and public health management. Working Group on Civilian Biodefense.
=============================================================
JAMA 1999 Jun 9;281(22):2127-37
Henderson DA, Inglesby TV, Bartlett JG, Ascher MS, Eitzen E, Jahrling PB, Hauer J, Layton M, McDade J, Osterholm MT, O'Toole T, Parker G, Perl T, Russell PK, Tonat K.
The Center for Civilian Biodefense Studies, School of Public Health, Johns Hopkins University, Baltimore, MD 21202, USA. [email protected]
OBJECTIVE: To develop consensus-based recommendations for measures to be taken by medical and public health professionals following the use of smallpox as a biological weapon against a civilian population. PARTICIPANTS: The working group included 21 representatives from staff of major medical centers and research, government, military, public health, and emergency management institutions and agencies. Evidence The first author (D.A.H.) conducted a literature search in conjunction with the preparation of another publication on smallpox as well as this article. The literature identified was reviewed and opinions were sought from experts in the diagnosis and management of smallpox, including members of the working group. CONSENSUS PROCESS: The first draft of the consensus statement was a synthesis of information obtained in the evidence-gathering process. Members of the working group provided formal written comments that were incorporated into the second draft of the statement. The working group reviewed the second draft on October 30, 1998. No significant disagreements existed and comments were incorporated into a third draft. The fourth and final statement incorporates all relevant evidence obtained by the literature search in conjunction with final consensus recommendations supported by all working group members. CONCLUSIONS: Specific recommendations are made regarding smallpox vaccination, therapy, postexposure isolation and infection control, hospital epidemiology and infection control, home care, decontamination of the environment, and additional research needs. In the event of an actual release of smallpox and subsequent epidemic, early detection, isolation of infected individuals, surveillance of contacts, and a focused selective vaccination program will be the essential items of an effective control program.
=============================================================
77.) A variant of variola virus, characterized by changes in polypeptide and endonuclease profiles.
=============================================================
Epidemiol Infect 1999 Apr;122(2):287-90
Dumbell KR, Harper L, Buchan A, Douglass NJ, Bedson HS.
St Mary's Hospital Medical School, University of London, UK.
A variant of variola virus is described which produces a late polypeptide of 25 kDa instead of one of 27 kDa and which has an additional endonuclease cleavage site for SalI in the viral DNA. These markers were shown to be genetically independent and to characterize 14 of the 48 variola strains which were examined. The variant strains were isolated from smallpox outbreaks originating in or from Pakistan between 1961 and 1974 and also from two cases at a Mission Hospital in Vellore, India in 1964. No variant strains were found among 9 other isolates from cases of variola major occurring in other parts of India or in Bangladesh, nor among 4 isolates from Indonesia, 15 from Africa or 6 isolates of variola minor.
=============================================================
78.) Eradication of vaccine-preventable diseases.
=============================================================
Annu Rev Public Health 1999;20:211-29
Hinman A.
Task Force for Child Survival and Development, Decatur, Georgia 30030, USA. [email protected]
Eradication is the permanent reduction to zero of the worldwide incidence of infection caused by a specific agent as a result of deliberate efforts; intervention measures are no longer needed. To date, the only infectious disease that has been eradicated is smallpox. Poliomyelitis is targeted for eradication by the year 2000, and the eradication initiative is well under way, with the Western Hemisphere certified as being polio-free and more than one year having passed since polio cases occurred in the Western Pacific Region of the World Health Organization. A review of the technical feasibility of eradicating other diseases preventable by vaccines currently licensed for civilian use in the United States indicates that measles, hepatitis B, mumps, rubella, and possibly disease caused by Haemophilus influenzae type b are potential candidates. From a practical point of view, measles seems most likely to be the next target. Global capacity to undertake eradication is limited, and care must be taken to ensure that a potential measles eradication effort does not impede achievement of polio eradication. Even in the absence of eradication, major improvements in control are both feasible and necessary with existing vaccines. New and improved vaccines may give further possibilities of eradication in the future. Eradication represents the ultimate in sustainability and social justice.
=============================================================
79.) President revokes plan to destroy smallpox.
=============================================================
Science 1999 Apr 30;284(5415):718-9
Marshall E.
Publication Types:
News
=============================================================
=============================================================
80.) Re-emergence of monkeypox in Africa: a review of the past six years.
=============================================================
Br Med Bull 1998;54(3):693-702 Related Articles, Books
Heymann DL, Szczeniowski M, Esteves K.
Division of Emerging and other Communicable Diseases Surveillance and Control, World Health Organization, Geneva, Switzerland.
Human monkeypox was first identified in 1970 in the Democratic Republic of the Congo. Extensive studies of this zoonotic infection in the 1970s and 1980s indicated a largely sporadic disease with a minority of cases resulting from person-to-person transmission, rarely beyond two generations. In August 1996, an unusually large outbreak of human monkeypox was reported, and cases continued through 1997 with peak incidence in August 1996, March 1997 and August 1997. Preliminary results from the field investigations in 1997 suggest a new epidemiological pattern where a majority of secondary cases result from person-to-person transmission, and a clinically milder disease. But there is preliminary laboratory evidence of a simultaneous outbreak of varicella in the same geographic region which will undoubtedly modify these preliminary results. Since smallpox was eradicated and vaccinia vaccination terminated in this region, the population of susceptible individuals has grown. The use of vaccination to protect the population at risk, however, must take into account HIV prevalence and the risk of generalized vaccinia when using vaccinia vaccine in populations where HIV is known to be present.
=============================================================
81.) Scientists split on US smallpox decision.
=============================================================
Nature 1999 Apr 29;398(6730):741
Comment in:
Nature. 1999 Jun 17;399(6737):632
Wadman M.
Publication Types:
News
=============================================================
=============================================================
82.) Smallpox preservation advisable.
=============================================================
Nature 1999 Apr 29;398(6730):733
Publication Types:
Editorial
=============================================================
=============================================================
83.) The major epidemic infections: a gift from the Old World to the New?
=============================================================
Panminerva Med 1999 Mar;41(1):78-84
Sessa R, Palagiano C, Scifoni MG, di Pietro M, Del Piano M.
Interdivisional Centre for Social Diseases, Faculty of Medicine and Surgery, La Sapienza University, Rome, Italy.
With the discovery of the New World, the Europeans flocked to America and with them spread infectious diseases. During long sea voyages the agents of these diseases increased their diffusion capacity in a suitable environment. Lack of hygiene, fatigue and privations, a diet without vitamins and many persons kept in confined spaces were the essential features of this environment. Sick persons, whose health conditions worsened during the journey to the New World, carried the germs of infectious diseases. The first disease to appear in the New World was smallpox described in 1518 in Hispaniola. From there the disease moved rapidly to Mexico in 1520, exterminating most of the Aztecs, Guatemala and to the territories of Incas from 1525-26, killing most of them and the King himself. The second disease, influenza, appeared in La Isabela, a few years later, causing a heavy epidemic between 1558 and 1559. Other diseases followed such as yellow fever and malaria. So Europeans and these invisible and mortal agents caused enormous destruction of American populations. In fact historians have estimated that beginning from early 1500, in only 50 years the population of Peru and Mexico fell from 60 to 10 million; in the latter country, in one century, the populations fell from an initial 10 million to only 2 million.
=============================================================
84.) New technologies for vaccines.
=============================================================
Wien Klin Wochenschr 1999 Mar 12;111(5):199-206
Dorner F, Eibl J, Barrett PN.
Biomedical Research Center, Baxter Hyland Immuno, Orth/Donau, Austria. [email protected]
The impact of vaccination on the health of the world's people has been considerable. With the possible exception of clean water, no other development has had such a major effect on mortality reduction and population growth. During the last 200 years vaccination has controlled nine major diseases and has led to the eradication of one, i.e. smallpox. However, in many instances, the exact mechanisms of successful vaccines are not fully understood. Almost all of the vaccines in use today are of three types: live attenuated microorganisms, inactivated whole microorganisms, or split or subunit preparations. These have different strengths and weaknesses with respect to safety and efficacy, but traditional vaccine development methodologies have not yet led to the generation of a vaccine with all the characteristics required of the ideal vaccine. Thus the development of improved vaccines that overcome the difficulties associated with many of the currently available vaccines is a major goal of biomedical sciences. In addition, there is an urgent need for new vaccines against the many infectious agents that still cause considerable morbidity and, in some cases, mortality. As has been the case in many areas of biology, the application of recombinant DNA approaches to vaccinology has opened up whole new areas of possibilities. The details of these and other technologies and their application to vaccine development are described in this review.
=============================================================
85.) Aftermath of a hypothetical smallpox disaster.
=============================================================
Emerg Infect Dis 1999 Jul-Aug;5(4):547-51
Bardi J.
Johns Hopkins University, Baltimore, Maryland, USA
The second day of the symposium featured a discussion of a scenario in which a medium-sized American city is attacked with smallpox. Four panels represented various time milestones after the attack, from a few weeks to several months. Panelists discussed what they and their colleagues might be doing at each of these milestones. The goal of the responses was to communicate the complexity of the issues and to explore the diverse problems that might arise beyond the care and treatment of patients.
The scenario itself was a step-by-step account of a smallpox epidemic in the fictional city of Northeast. Tara O'Toole, the scenario's lead author, read the narrative account before each panel.
The panelists responded to the events as if the epidemic were real and they were actually trying to identify, contain, communicate, and otherwise deal with it. Panel members included experts on hospital, city, state, federal, and media responses. Representing the hospitals were John Bartlett and Trish Perl, Johns Hopkins Hospital; Julie Gerberding, Hospital Infections Program, Centers for Disease Control and Prevention; and Gregory Moran, Emergency Medicine, University of California at Los Angeles. Jerome Hauer represented New York City's response. Representing the state were Michael Ascher, California Department of Health Services Laboratory; Arne Carlson, former governor of Minnesota; Terry O'Brien, a Minnesota State Assistant Attorney General; and Michael Osterholm, Minnesota Department of Public Health. The federal representatives on the panels were Robert Blitzer, former counterterrorism chief with the Federal Bureau of Investigation; Robert DeMartino, Substance Abuse and Mental Health Services Administration; Robert Knouss, Office of Emergency Preparedness, Department of Health and Human Services; and Scott Lillibridge, Centers for Disease Control and Prevention. Joanne Rodgers, Johns Hopkins Medical Institutions Public Affairs, spoke to the response of the media. George Strait, the medical news director for ABC News, acted as moderator for each of the panels scheduled on day two. D.A. Henderson also helped to moderate.
Identifying the Agent
At the start of the epidemic, 2 weeks after the bioterrorist attack, confusion reigns. There is uncertainty as to what the infection is and reluctance to diagnose smallpox even when it is suspected. It is unclear who is in charge of investigating and containing the epidemic. Outside, reporters are knocking on the hospital doors. The question of what took so long to identify the agent opens the panel. Smallpox, a nonspecific flulike illness, is hard to diagnose, replies an emergency medicine physician. The disease is not suspected because it was eradicated in the late 1970s. Any laboratory work on the first cases would initially be testing for a battery of other causes, such as other viral infections (e.g., monkeypox) or reactions to recent vaccinations. A window of 2 weeks before positive identification of smallpox may even be optimistic. The diagnosis would probably take much longer because of physicians' lack of familiarity with the disease.
When all the tests for other infections turn up negative and smallpox is strongly suspected, suggests a state laboratory chief, a conclusive result from the laboratories at the Centers for Disease Control and Prevention (CDC) or the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) would still be needed. These are the only two places in the United States equipped to identify smallpox virus in tissue samples. This part of the diagnosis is fairly straightforward but it would take at least 1 day before the definitive results could be obtained.
Responding at the Hospital Level
Hospitals would probably isolate the early cases presumptively, even if smallpox was not suspected, since the symptoms would appear infectious. This is the opinion of a hospital infections expert. In the city, argues a state health department professional, several hospitals would each see one or two of the first few cases. The city health department would quickly become aware of the similarity of the cases in the various hospitals, recognize a potential outbreak (probably measles) and mobilize early to contain it.
Once smallpox is identified, the following organizations within city government would be notified: the police department, the local emergency management office, the city health commissioner's office, and, ultimately, the mayor's office. This process may be difficult since it requires integrating the health department into emergency management plans, an event with little precedent, notes a city emergency official.
Coordinating Response Efforts
Who is in charge, agree panelists, is one of the most important questions yearly in the epidemic, because any large-scale relief effort would require good management. Complicating the answer, however, are various levels of government, each with its own responsibilities and perspective on response, as reflected in panelists' remarks.
Acts of domestic terrorism are under the jurisdiction of the federal government, so several federal agencies become involved, starting with FBI. FBI is involved from the very beginning since any cases of smallpox would indicate a deliberate terrorist attack. A criminal investigation begins immediately. CDC is involved as soon as samples are sent for laboratory diagnosis.
The state government becomes involved at the outset, since major threats to public health are dealt with on the state level. The state health department starts its own investigation, and to reassure the public, the governor may act as a spokesperson for the management of the epidemic.
The city is involved from the outset, explains the city emergency management official, understanding that "bioterrorism is a local issue," which escalates very rapidly to state and federal levels. The local police and emergency management teams, as well as the city health commissioner, the city health department, and the mayor, are involved.
The problems of the city become state problems immediately, counters the former governor, because the news media treat any potential infectious disease outbreak as a regional problem. This forces the governor's hand. The governor has to move in because there is a need for one person to be in charge.
The most difficult situation is how to deal with the hospital patients. One danger in the early days is losing control of the crisis through panic. Once rumors about smallpox start to spread, many workers within the hospital walk off the job. Understaffing also leads to increased stress and confusion for patients and providers alike.
Even before federal and state command structures are in place, suggests a hospital infections control expert, hospital epidemiologists would already be addressing infection control issues. She notes that hospital infection control specialists would be on the phone to colleagues in other city hospitals alerting one another. Hospital epidemiologists, adds a state health official, would have a contact list of state, local, and federal public-health authorities who also would be notified.
Another problem in coordination becomes clear to panelists: the difficulty in sharing classified risk information among agencies and various levels of government. Any early warning, which could have contributed to a more effective response, was missing in the scenario. Even though the FBI had some early intelligence of the attack, the alerting of health care workers was nonexistent. The problem lies in the fact, assesses a state health department official, that health departments have never been seen as intelligence communities, nor has there ever been a precedent for passing such information to them.
On the federal level, CDC addresses the public health issues of the epidemic, and FBI addresses the law enforcement issues. These aims are not necessarily exclusive of one another, and the possibility of linking efforts is raised. Everyone interviewed as a part of the epidemiologic investigation may have to be interviewed as part of the criminal investigation as well. Perhaps the most effective way to accomplish this is to conduct both interviews simultaneously.
Some aspects of the two federal agencies may overlap, perhaps even conflict, in agendas. Specimens that are sent to CDC for positive identification of the smallpox virus may be needed by FBI as evidence for any eventual prosecution. In many ways, it may appear as if FBI is running the investigation. However, dealing with the sick, obtaining vaccine, and mobilizing the epidemiologic investigation at the local, state, and federal levels are outside the scope of FBI. CDC takes the lead on these public health issues, and together with FBI, coordinates the management of federal resources.
However, who is coordinating activities at the hospitals is still unclear, and the question of authority on that level is unresolved. Can outsiders come into a hospital and wield power, and if so, who are they? Federal responders may have ambiguous authority within a hospital and may add to the chaos. An FBI offical notes that his agency's role in the hospitals will simply be to inform the doctors and administrators of what the hospital needs to do to assist in the criminal investigationkeeping evidence and coordinating interviews with patients. However, this may still leave gaps of authority within the hospital.
In the scenario under consideration, the state identifies one hospital as the smallpox hospital, and this also presents a problem of coordination. The hospital itself has to work out the details of local quarantine and the distribution of medicine to the patients, and there is a need to protect the health-care workers and other hospital staff. Vaccine should be immediately available to these workers, and its distribution will have to be coordinated with CDC.
Outside the hospitals, an epidemiologic investigation will be taking place that will need to be coordinated with CDC. A CDC official points out the need for surveillance in the early days of the epidemic. To assist in collecting data necessary to identify the release source and people at risk, he recommends that CDC provide additional staff for much of the epidemiologic work, including mid- and senior-level investigators. Bringing in these outside experts should not represent a problem for local officials, he suggests, since CDC already has strong ties with state epidemiologists.
Informing the Public
How to control the message going to the public weighs heavily upon the minds of all panelists. Reporters on the hospital scene will quickly become aware of any rumors and will demand answers of any worker or official who is handy. Official channels will not be the only source of information during the epidemic, argues the public affairs specialist.
First responders, such as the police or fire officials, might show up with full biohazard protection; such an image immediately raises questions. The media will digest information from day one, whether or not there is an official statement from the city, state, or federal level.
Controlling the message that goes out over the airwaves could be extremely difficult, especially since there may not even be any consensus on what the message should be in the first place. Several panelists point out the need to ensure that information presented to the media is consistent and credible. The city emergency manager suggests that the mayor will work with federal and state officials to get consistent and credible information out to the public. One viable alternative to speculation and misinformation, proposes an FBI official, is to have a centralized joint information center, such as the one his agency set up in Oklahoma City after the bombing, with several experts answering all the questions that arise.
Regardless of how information is disseminated, the message must be carefully considered. If the flulike symptoms of smallpox are identified on the evening news, a flood of noninfected persons with stuffy noses or headaches could swell emergency rooms across the state. Other reports, such as upcoming quarantine efforts, may also spread panic and should be handled carefully. The types of stories the media choose to write present a challenge. The press will not only cover the crisis but the managers of the crisis. Plans for responding to questions about crisis management must be in place. Whether or not the message that goes out to the public includes mention of terrorism should be weighed.
The hospital infections expert pursues a different angle to the issue of information exchange. The difficulties in interviewing the public have not been solved, she points out. Who will do the interviews? How they will be coordinated with criminal investigations? Who will receive vaccine? And how will health-care workers be protected? Will the system be overwhelmed by false casespeople who think they have smallpox? Moreover, a basic problem in the early days of the epidemic is the need for an infrastructure to handle the large volume of calls flooding the hospitals.
Handling Logistics
What will be the plan of action? Hundreds of people will have to be mobilized to interview the public, and hundreds more will be needed to administer vaccine. The distribution of antibiotics and vaccines represents a logistical problem that must be overcome.
As the epidemic grows and spreads to several states, friction between the levels of government grows. Governors are demanding vaccine supplies, fueling a larger debate of how vaccination should be handled. Tens of thousands of people are vaccinated, but many more still need vaccine. Media reports begin to be critical of the government's handling of the crisis.
What still needs to be done? With a growing number of deaths, the rise in the number of patients in quarantine, the loss of critical health-care workers and city emergency workers, within the city things are beginning to get out of focus, notes a city official. Asking how leadership will function inside the hospital, the hospital epidemiologist identifies a need for official responses that are well thought out, strong, and based on hard science.
The vaccine campaign poses significant issues. The limited supply of vaccine must be divided up and distributed according to greatest riskpersons who may have been infected or who care for those infected, argues an official in federal emergency management. Political leaders and essential city workers are other priority groups. A consensus must be reached as to how to proceed with the vaccinations. CDC is best suited to coordinate vaccine efforts, but the public health community must work towards an emergency. The governor, warns the city emergency manager, may step in and call the shots. There is a need for a public health emergency plan. Did the outbreak start from a single source or from multiple sources? This determination would help with vaccine management and allocation, but there is no answer. Moreover, testing facilities at CDC and USAMRIID are overwhelmed at this point in the epidemic.
Hospitals must deal with quarantine. Restrictions are imposed in the first days or weeks of an epidemic. Workers' fear of being sequestered causes them to leave hospitals understaffed. Many people are likely to stay at their posts if they feel they have reliable information and support, argues a mental health provider. Some, however, may leave the front lines to go home to their own families.
Legal Ramifications
According to a 1905 Massachusetts case, cites a state's assistant attorney general, compulsory vaccinations are not a violation of due process and are therefore legal. So the local, state, and federal levels of government have no obstacle to vaccinating those designated at risk.
A more difficult legal question is that of quarantining smallpox patients. Many of the public health codes used to allocate powers to government officials are old and may not be valid or useful. Also, court precedents from HIV cases may have heavily weighted matters in favor of due process. Minnesota, for example, requires a separate court hearing for each case of quarantine. Thus, quarantine may be possible in a hospital but not in the community.
Another basic legal question is whether the lines of legal support are clear to all officials, such as hospital guards and police officers. How far can police go to detain quarantined patients? The limits of emergency powers should be clearly delineated in any predisaster planning.
The epidemic is threatening to expand beyond the city into the rest of the country and even beyond. The World Health Organization (WHO) will probably become involved, and travel notifications have to be introduced.
Vaccine Supply
Even without adequate supplies of vaccine, much can be done with the existing stocks. Prevaccinating some health-care workers is a proactive approach. Having a sizable pool of prevaccinated professionals who can mobilize and act as emergency responders takes much of the pressure off local hospitals. One way to reduce secondary transmission (outside of vaccinating the contacts of the infected person), instructs the hospital epidemiologist, is good infection controlwearing filter masks and washing hands well. Another way of controlling the epidemic is through quarantine. While these measures are not a substitute for adequate vaccine supply, they can slow the epidemic.
One problem with the vaccine supply is that many more people want to be vaccinated than limited stores permit. There are not even enough stores of vaccine to prevent the spread of the epidemic. The existing 6 to 7 million doses of smallpox vaccine will not last forever, and the 36 months it takes for additional large-scale preparations is prohibitive, argues a vaccine campaign expert. Health officials will likely not have the time or resources to target precisely those people who have an actual need for vaccine. The need for vaccine will overwhelm the supply.
The cost of vaccine development may inhibit stockpiling, proposes a CDC official. Since an attack with smallpox is of low probability, large-scale production may be difficult to justify. A partnership between private industry and the government would help, however. Also, the cost of getting caught without an adequate supply could be disastrous.
Possible emergency measures to stretch the vaccine supply, proposes a smallpox expert, include arm-to-arm vaccination as pustules form on the arms of vaccinated people; vaccinia could be grown in massive amounts in tissue culture; and 30 million doses of vaccine could be contracted from South Africa.
The Final Stage
The smallpox epidemic has become a major public health emergency affecting several cities in many states and at least four other countries. The event is identified as a terrorist attack, because no other source of smallpox outside a deliberate release exists. For those who have already contracted smallpox, antiviral drugs, such as cydolfivir, may be useful but these medicines may be just as scarce as the vaccines.
Secondary transmission got out of hand, vaccine use did not contain the epidemic, and standard planning did not work. Thus a state health official sums up the deficiencies of response. Hospital resources have been overwhelmed, with people flooding emergency rooms in the belief they have smallpox. These cases are added to hospitalized cases before and during the epidemic; yet there are not even enough beds for all the sick. The hospital staff have become physically and emotionally exhausted from the long hours and from seeing about a third of infected patients die.
Failure of containment has turned the outbreak from local to national and international. However, the epidemic would have been much worse, had it gone unchecked, notes a state health official. Containment was significant. The 15,000 smallpox cases could have easily been more than 100,000.
No perpetrators have yet been identified, despite combining the criminal and the epidemiologic investigations. Such methodical work, however, is important because, unless the intelligence community comes up with information or a tip, there is no other way to identify the source of the epidemic, explains an FBI offical.
Many of the problems in the epidemic could have been avoided or controlled if extensive plans had existed, panelists agree. The panelist speaking from a governor's perspective identifies leadership as the most pressing void. Should the city have been placed under immediate quarantine? Should martial law have been implemented? Is the designation of a single smallpox hospital a reasonable thing for any city to do? These are difficult questions to face in the wake of a disaster. Such issues must be addressed long before trouble strikes.
Who Will Pay for the Smallpox Epidemic?
The significant cost of curtailing the epidemic is debated. How will a smallpox hospital be financed, inquires a physician. The money might come from the federal government as emergency management funding, suggests a city emergency manager. The infrastructure and linkages within the public health community could be improved, the capacity for laboratory testing of samples could be increased, surveillance methods could be enhanced, and a health information strategy could be developed.
While the smallpox scenario is certainly frightening, experience with earlier epidemics (smallpox among them), knowledge of the issues, and expertise to deal with them show that in a crisis people from all disciplines pull together.
Mr. Bardi is a freelance writer in Baltimore who holds degrees in biophysics and science writing from Johns Hopkins University.
Address for correspondence: Jason Bardi, Johns Hopkins University, Center for Civilian Biodefense Studies, 111 Market Place, Ste. 850, Baltimore, MD 21202, USA; fax 410-223-1665; [email protected].
Johns Hopkins University, Baltimore, Maryland, USA. [email protected]
=============================================================
86.) Strengthening National Preparedness for Smallpox: an Update
=============================================================
Current Issue
Vol. 7, No. 1
Jan–Feb 2001
Research Update
James W. LeDuc* and Peter B. Jahrling†
*Centers for Disease Control and Prevention, Atlanta, Georgia, USA; †United States Army Medical Research Institute of Infectious Diseases, Fort Detrick, Frederick, Maryland, USA
Concern that smallpox virus may be used as a biological weapon of mass destruction has prompted calls for production of additional vaccine and new research into variola virus diagnostics and clinical interventions. Only 15.4 million doses of smallpox vaccine, produced approximately 20 years ago, exist in the United States (1). While virtually all lots remain potent, additional vaccine would clearly be needed in a national emergency involving smallpox virus. Global eradication of natural smallpox disease was declared in 1980; with eradication, most research activities involving the virus ended. Although the complete genomic sequence of selected isolates of variola virus is known (2), the diagnosis and treatment of smallpox infection have not changed in the past two decades. Recognizing the need for advancement in these areas before variola virus stocks are destroyed, the World Health Organization (WHO) passed a resolution (WHA 52.10) in 1999 extending the date of destruction of all remaining variola virus stocks until the end of 2002. The midpoint of this period is an appropriate time to review progress made in vaccine production and variola virus research and to outline the next steps.
Vaccine Production
On September 20, 2000, the Centers for Disease Control and Prevention (CDC) entered into an agreement with OraVax (Cambridge, MA) to produce a new smallpox vaccine. Like the vaccine used to eradicate smallpox, the new vaccine will contain live vaccinia virus; however, it will be produced in cell cultures by modern vaccine production techniques. OraVax will coordinate full clinical testing of the vaccine and submit a licensing application to the U.S. Food and Drug Administration (FDA) for the prevention of smallpox in adults and children. Forty million doses of the new vaccine will be produced initially, with anticipated delivery of the first full-scale production lots in 2004. The agreement calls for sustained annual production through 2020 to replace outdated vaccine and allows for increased production should an emergency arise. The vaccine will be administered with bifurcated needles (also produced by OraVax), which create a localized vaccine "pock" and confer protective immunity. The vaccine will be held in reserve as part of the national stockpile and be released only in the event of a confirmed case of smallpox or when vaccination against vaccinia virus is warranted. The agreement allows OraVax to produce additional vaccine for other markets, including international buyers.
Variola Virus Research
A research plan, implemented at CDC by scientists from both the Department of Defense and CDC and including extensive collaborations with scientists from the National Institutes of Health and other organizations, is being undertaken with WHO concurrence. All work with live variola virus is done under biosafety level 4 containment conditions at CDC. Smallpox virus is officially retained at only two facilities in the world: at CDC in the United States and the State Research Center of Virology and Biotechnology in Novosibirsk, Russia. Research teams from both institutions are coordinating activities to avoid duplication and gain the maximum amount of information possible before final destruction of the virus.
Strain Evaluation
Of 461 isolates in the smallpox virus collection at CDC, 49 were selected for further characterization. These isolates, which included both variola major and variola minor, were selected to represent the greatest diversity in date of collection and geographic region. Of the 49 isolates tested for viability, 45 were successfully recovered, and seed stocks were prepared for subsequent studies. This group of 45 represented isolates from as early as 1939 and as late as the 1970s; all major geographic regions were represented. Study of these isolates is based on three research themes: application of modern serologic and genomic methods in the diagnosis of variola virus disease; determination of candidate antiviral drug activity against this virus; and investigation of the pathogenesis of smallpox infection, especially through the development of a nonhuman primate model to replicate human smallpox infection. The research team carefully outlined all experimental work to be undertaken with variola virus, incorporating suggestions from a peer group of highly qualified external experts from academia and industry; the first set of experiments was conducted from January to July 2000 in the CDC maximum containment laboratory.
Serologic Assays
Because enzyme immunoassay technology was still in its infancy when smallpox was eradicated, during the first series of experiments, polyclonal and monoclonal antibodies had to be produced for developing enzyme-linked immunosorbent assays to measure variola virus-specific immunoglobulin (Ig) M, IgG, and antigen. These reagents are now being evaluated by prototype assays with inactivated viral antigens. This work will continue for the foreseeable future.
Nucleic Acid-Based Diagnostics
Viral DNA was extracted from all 45 successfully recovered isolates, was purified and inactivated, and is now being examined by restriction fragment-length polymorphism developed by an extended polymerase chain reaction assay that amplifies viral genome into 20 overlapping products of approximately 10 kilobases each. These products cover virtually the entire length of the viral genome and include sequences in essential genes and genes likely needed for pathogenesis. Preliminary results indicate that the data thus generated offer a good low-resolution overview of genetic diversity of variola viruses and are being used to differentiate strains, infer phylogeny, and identify as many as 10 additional variola isolates for complete genome sequencing. Two isolates, Somalia 77 and Congo 70, were specifically suggested by WHO for sequencing, and this work has begun. A dedicated sequence and bioinformatics facility being developed at CDC will be used to undertake this effort and to begin constructing a genomic signature database, not only for smallpox but also, over time, for other pathogens with bioterrorism potential.
Antiviral Drugs
Two hundred seventy-four antiviral drug compounds were screened for activity and therapeutic indices against variola, monkeypox, cowpox, camelpox, and vaccinia viruses by two cell culture assays. Many of these compounds were provided for testing under collaborative arrangements facilitated by an orthopox antiviral research initiative of the National Institute of Allergy and Infectious Diseases. Previous studies identified a nucleoside phosphonate DNA polymerase inhibitor, cidofovir (Vistide), as being active against poxviruses, including variola. In the current trial, cidofovir and its prodrug (cyclic HPMPC) were evaluated against 31 strains of variola, which were selected to cover a wide geographic area and time span. No substantial differences in inhibition among strains were observed, which suggests that cidofovir-resistant strains are unlikely. The in vitro inhibition was further characterized in multiple cell lines to meet FDA requirements. However, another class of antiviral drugs, the S-adenosylhomocysteine hydrolase inhibitors, showed considerable variation in the 50% inhibitory dose between variola isolates; this effect should be investigated further.
Two approaches to the development of an oral prodrug of cidofovir yielded compounds with improved antiviral activity. In addition, the current series of experiments identified 27 other compounds, including completely new classes of drugs, that appear to be active against variola and other orthopoxviruses. In fact, 10 compounds had therapeutic indices greater than 200, while cidofovir had indices greater than 10; 3 compounds had therapeutic indices greater than 1,500. When work resumes in early 2001 with live variola virus, we will continue to evaluate these and additional compounds for activity, including analogs designed for oral administration. The most promising compounds emerging from this in vitro testing will be evaluated in animal models, e.g., cowpox and vaccinia in mice and eventually monkeypox virus challenge in nonhuman primates. All promising compounds will be tested against a battery of surrogate orthopox viruses to guide evaluation of new antiviral compounds after variola virus is no longer available.
Animal Models
A major goal of the current research is to define an animal model that faithfully replicates human smallpox. Such a model would be extremely valuable in evaluating candidate antiviral drugs and novel diagnostic assays and in defining the pathogenesis of smallpox. Consequently, two groups of four cynomolgus macaques were exposed to two variola virus strains at a high dose (>108 PFU) by the aerosol route. Clear evidence of infection was found; the animals had transient fevers, perturbations in cytokine titers in serum, and mild exanthemous lesions. A few of the monkeys showed signs of bronchopneumonia, but none died or had disease similar to the classic smallpox seen in humans. Another series of experiments will be undertaken with different variola isolates to confirm these preliminary observations and generate additional clinical material to validate the diagnostic assays under development.
The results of the research now under way, coupled with the promise of renewed production of smallpox vaccine, will better prepare the United States--and indeed the entire world--for the possibility that smallpox virus might be used as a terrorist weapon of mass destruction.
James W. LeDuc* and Peter B. Jahrling†
*Centers for Disease Control and Prevention, Atlanta, Georgia, USA; †United States Army Medical Research Institute of Infectious Diseases, Fort Detrick, Frederick, Maryland, USA
References
LeDuc JW, Becher J. Current status of smallpox vaccine. Emerg Infect Dis 1999;5:593-4.
Shchelkunov SN, Massung RF, Esposito JJ. Comparison of the genome DNA sequences of Bangladesh-1975 and India-1967 variola viruses. Virus Res 1995;36:107-18.
=============================================================
87.) Smallpox: An Attack Scenario
=============================================================
Tara O'Toole
Johns Hopkins School of Public Health, Baltimore, Maryland, USA
Smallpox virus, which is among the most dangerous organisms that might be used by bioterrorists, is not widely available. The international black market trade in weapons of mass destruction is probably the only means of acquiring the virus. Thus, only a terrorist supported by the resources of a rogue state would be able to procure and deploy smallpox. An attack using the virus would involve relatively sophisticated strategies and would deliberately seek to sow public panic, disrupt and discredit official institutions, and shake public confidence in government.
The following scenario is intended to provoke thought and dialogue that might illuminate the uncertainties and challenges of bioterrorism and stimulate review of institutional capacities for rapid communication and coordinated action in the wake of an attack.
Capacity To Detect a Bioterrorist Attack and To Diagnose an Unusual Disease
April 1
The vice-president visits Northeast, a city of 2.5 million. His itinerary includes an awards ceremony, an appearance at a local magnet school, and a major speech at the local university. A crowd of 1,000 people, including students, is gathered in the university auditorium. Hundreds more wait outside, where the vice-president stops to shake hands and respond to queries from the media.
The Federal Bureau of Investigation (FBI) has information suggesting a possible threat against the vice-president from a terrorist group with suspected links to a rogue state. The group is known to have made inquiries about acquiring biological pathogens, including smallpox, and is suspected of having procured aerosolization equipment. FBI decides its information is too vague and too sensitive to pass on to the Department of Health and Human Services, local law enforcement authorities, or the state health department.
April 8
FBI informants report rumors that something happened while the vice-president was in Northeast.
April 12
A 20-year-old university student goes to the university hospital emergency room with fever and severe muscle aches. She is pale, has a temperature of 103°F, and is slightly leukopenic, but the physical exam and laboratory results are otherwise normal. She is presumed to have a viral infection and is sent home with instructions to drink fluids and take aspirin or ibuprofen for muscle aches. Later that day, a 40-year-old electrician arrives at the emergency room with severe lower backache, headache, shaking chills, and vomiting. He appears pale and has a temperature of 102°F and a pale erythematous rash on the face. The patient is a native of Puerto Rico, where he visited 10 days earlier. A diagnosis of dengue fever is considered, and the patient is discharged with ibuprofen and instructions to drink fluids.
April 13
Over the course of the day, four young adults in their twenties come to the university hospital emergency room with influenzalike symptoms and are sent home.
April 14
The female student returns to the emergency room after collapsing in class. She now has a red, vesicular rash on the face and arms and appears acutely ill. Her temperature is 102°F; her blood pressure is normal. She is admitted to an isolation room with presumptive diagnosis of adult chickenpox. She has had no contact with others known to have chickenpox.
April 15
The electrician first seen on April 12 returns to the emergency room by ambulance. He too has a vesicular rash and appears very ill. He is also admitted to an isolation room with presumptive diagnosis of chickenpox.
That evening at 6 p.m. the infectious disease consultant and the hospital epidemiologist meet on the elevator. The infectious disease specialist has just finished examining the student and the electrician, both of whom have vesicular rash on the face, arms, hands, and feet. The skin lesions are evolving in phase. The possibility of smallpox is raised. The infectious disease specialist takes a swab specimen from the electrician's skin lesions, sends it to the laboratory, and requests that it be examined by electron microscopy by an experienced technician. The doctor assures the technician that he will be vaccinated if the specimen shows smallpox. At 7:00 p.m., electron microscopy shows an orthopoxvirus consistent with variola—the smallpox virus.
At 7:15 p.m. the hospital epidemiologist declares a contagious disease emergency. The two patients are moved to negative-pressure rooms with HEPA filters. Visitors and hospital staff not already caring for and in contact with patients are forbidden to enter the floor. Infection-control nurses begin interviewing staff to determine who has been in face-to-face contact with the patients during initial emergency room visits and admission. The hospital epidemiologist calls the chair of the department of medicine and the hospital vice-president for medical affairs.
Within 45 minutes the chair of the department of medicine and the president of the hospital are meeting with the infectious disease physician, the hospital epidemiologist, the hospital vice-president for public relations, and the hospital's general counsel. The city and state health commissioners join the meeting by phone. The need to vaccinate and isolate all contacts of the patients is recognized and discussed. It is decided to secure the hospital. No one is allowed to leave until all persons are identified so that they can be vaccinated as soon as vaccine can be obtained from the Centers for Disease Control and Prevention (CDC). The possibility of identifying and vaccinating other patient contacts (e.g., family members not now in the hospital) is discussed, but no decisions are made because the hospital's legal authority for doing this is unclear.
Half an hour later, the state health commissioner calls FBI. He also contacts CDC to request that smallpox vaccine be released for hospital staff and patient contacts. Because vaccine supplies are limited, CDC requests that the diagnosis of smallpox first be confirmed at CDC. CDC calls FBI and arranges to fly a three-person Epidemic Intelligence Service team to Northeast for assistance.
By 9:30 p.m., an FBI special agent arrives at the hospital, secures biological samples taken from the patients, and drives them to Andrews Air Force Base, where a military aircraft flies the samples to CDC's Biosafety Level 4 laboratory in Atlanta, Georgia. FBI requests that city police be called to help maintain order and ensure that no patients, staff, or visitors leave the hospital until all occupants have been identified and their addresses have been recorded. More FBI agents and city police arrive on the hospital grounds.
Hospital visitors are confused and angered by police refusal to allow anyone to leave the hospital. No explanation is given for the containment to staff, visitors, or the police. Ambulances are rerouted to other hospitals. The rumor that smallpox has broken out rapidly spreads through the building, as do rumors that a terrorist wanted by FBI is in the building. A fight erupts between people trying to leave the facility and the police. Three people are injured and sent to the emergency room. More police and FBI agents arrive and surround the building.
The local television networks report the scene outside the hospital on the late night news. The hospital public relations representative explains that the lock-in is temporary and intended only to gather names and addresses so that people can be contacted and treated if a suspected, but unnamed, contagious disease is confirmed. CNN arrives and demands access to the hospital and affected patients. Rumors about what the contagious disease might be include Hong Kong flu, meningitis, Ebola virus, smallpox, and measles.
The mayor and state attorney general's office are contacted by the health commissioner. There is a phone discussion with the hospital's general counsel and epidemiologist about the right to impose quarantine. Visitors, nonessential personnel, and new patients are blocked from entering the hospital, but visitors already in the building are allowed to leave after their names and addresses are recorded.
FBI, however, is reluctant to allow anyone to leave the building. This provokes a lengthy exchange among the FBI agent-in-charge, the city police chief, and hospital administrators and attorneys. The dispute is resolved after a series of phone calls between FBI headquarters and the state attorney general's office.
Early Response
11:30 p.m.
The specimen arrives at CDC. At midnight, the diagnosis of smallpox is confirmed. A phone conference with hospital staff, the city police chief, the state health commissioner, the state attorney general, the governor, CDC, FBI, an assistant secretary of the Health and Human Service (HHS), and staff from the National Security Council and the White House (32 people in all) focuses on whether and how to release the information to the media. The mayor and the governor will go on television in the morning with the health commissioner. The FBI director will also make a statement. The president will address the country at noon.
CDC makes arrangements to release smallpox vaccine early the next morning for use by patient contacts and the health-care teams caring for hospitalized victims.
April 16
Morning conference calls between CDC, FBI, HHS, the National Security Council, and state health authorities are set up. Federal officials now assume that a bioterrorist attack has occurred in Northeast. There is concern that other attacks might also have taken place but not yet come to light or that further attacks might be imminent.
A representative from the counterterrorism office of the National Security Council asks if it is necessary or desirable to attempt a complete quarantine of Northeast, including closure of the city airport and a ban on rail traffic leaving from or stopping in the city. The group agrees that such a step is neither feasible nor warranted. A heated debate follows about the advisability of vaccinating all hospital staff and visitors at all facilities where a single case of smallpox is clinically suspected. The state health commissioner presses for enough vaccine for the entire city of Northeast.
FBI and CDC are reluctant to begin mass vaccination until the dimensions of the outbreak are better understood. It is decided to vaccinate all hospital staff and any visitors to the floor where the patients were located. All direct contacts of the patients will also be vaccinated. By the end of the long phone conference, the decision is made to vaccinate all health-care personnel, first responders, police, and firefighters in any city with confirmed cases of smallpox.
CDC Epidemic Intelligence Service officers arrive in Northeast to assist the state epidemiologist, who is establishing a statewide surveillance and case investigation system. Efforts begin to develop a registry of all face-to-face contacts of smallpox patients and to monitor, daily, all contacts for fever. Anyone who has fever >101°F is to be isolated, at home if possible, and be followed for rash.
The state health department activates a prearranged phone tree to query all hospitals and walk-in clinics in the state about similar cases and counsels immediate isolation of all suspected patients.
An additional eight admissions for fever and vesicular rash are discovered. All patients are extremely ill; two are delirious. The university hospital emergency room records are searched, and staff attempt to contact all patients who had fever during the previous week. Three more probable smallpox cases are discovered. Telephone follow-up reveals that one has been admitted to another hospital out of state.
CDC and state health officials discuss possible strategies for managing the epidemic if there is insufficient vaccine for all patient contacts, as seems likely. Home isolation of nonvaccinated patient contacts is considered, but the legal authorities, practical logistics, and ethical implications of such a strategy remain unclear and unresolved.
After discussion among state health authorities and university hospital staff, it is decided that the university will serve as the city's smallpox hospital and will accept transfers of smallpox patients now hospitalized at other facilities in the state. Other hospitals will refer patients to the university hospital or to the state armory but will not admit patients with suspected smallpox. Physicians will be urged to avoid seeking admission for most smallpox patients and to care for patients in their homes.
Arrangements are made by the state health commissioner to activate a state disaster plan, which establishes the armory as an emergency hospital for the quarantine of smallpox patients, in case the number of smallpox patients exceeds hospital isolation capabilities.
Quarantine and Vaccination
During the morning interagency phone conference, Department of Justice representatives raise questions about potential legal liabilities associated with adverse vaccine effects. The questions remain unresolved, but vaccination will proceed.
On the evening of April 16, the president goes on television to inform the nation of the bioterrorist attack by unknown terrorists, vows that the assailants will be identified and brought to justice, and urges calm and cooperation with health authorities.
The initial epidemiologic evidence and FBI information suggest that the smallpox release likely occurred during the vice-president's January speech at the university in Northeast. Efforts are begun to identify and vaccinate everyone who attended the speech. Additional health department personnel are detailed to help in the epidemiologic investigation. Media reports say that the government does not know how many people are sick or how widespread the outbreak might be.
By evening, 35 more cases are identified in eight emergency rooms and clinics around the city; 10 cases are reported in an adjoining state. CDC alerts all state health departments to be on alert for possible smallpox; CDC also urges prompt and strict isolation measures and instructs states to send specimens from suspected patients to its headquarters in Atlanta for definitive laboratory diagnosis.
April 17
In Northeast, 10,000 residents are vaccinated by the city and state health departments with assistance from volunteer physicians and nurses. Vaccination of the entire university student body, faculty, and staff is discussed and rejected by federal officials for fear that vaccine supplies will be needed for contacts of confirmed cases. State health officials continue to press for a statewide vaccination effort. Unions representing nurses and other health-care workers call for vaccination of all employees whose jobs involve direct patient contact.
April 18
An additional 20,000 residents of Northeast are vaccinated.
April 19
CDC and the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) determine that the infecting strain of smallpox was not bioengineered. The genomic sequence is entirely typical of known smallpox strains.
The student with the first diagnosed case dies. Ten more smallpox cases have been identified, bringing the number of confirmed cases to 50. The patients are located in four states, all in the mid-Atlantic area. Suspected cases are identified in five other states.
April 20
Governors of affected and unaffected states press, both behind the scenes and publicly, for emergency vaccine stocks to be distributed to states so that immediate action can be taken should an outbreak occur.
At the close of day 4 of the vaccination campaign, 80,000 have been vaccinated.
April 22-27
No new cases of smallpox with onset after April 19 have been confirmed, although many suspected cases with fever and rash due to other causes are being seen. In the states reporting confirmed smallpox cases, thousands of people are seeking medical care because of worrisome symptoms. CDC and state health authorities decide to issue a recommendation that patients with fever who cannot be definitively diagnosed be strictly quarantined and observed until the fever subsides. CDC and state health departments are flooded with calls from health-care providers seeking guidance on isolation procedures.
Some hospitals and health maintenance organizations (HMOs) complain to HHS that they cannot afford to isolate the many patients with fever and rash at their facilities and demand that the government pay quarantine costs. State health departments are similarly worried about the costs of quarantine.
Local media report an outbreak of sick children with rash in an area elementary school. It is unclear whether the illness is chickenpox or smallpox. Television stations show film of parents arriving at school in midday to remove children from classrooms. A college basketball star is rushed to hospital by ambulance with an unknown illness. Local television reports that the athlete has high fever but no rash. Both stories are covered on the national evening news.
April 28
Smallpox is diagnosed in two young children in Megalopolis, a large city in another state. FBI and the National Security Council worry that these cases might signal another attack since the children have had no discernible contact with a smallpox patient or contacts. The possibility that there has been a new attack is weighed against the possibility that the children were infected by a contact of one of the first wave of patients who was missed in the epidemiologic investigation.
Members of the state congressional delegation demand that the federal government implement a massive citywide vaccination program. CDC notes that a Megalopolis-wide vaccination program would deplete the entire civilian vaccine supply.
The media report that the president, vice-president, cabinet representatives, and prominent members of Congress have been vaccinated, and the military has already begun to vaccinate the troops in affected states and Washington, D.C.
The Epidemic Expands
April 29
Over the course of the day, CDC receives reports of an additional 100 new cases of potential smallpox. Sixty of these are in the original state. The others are scattered over eight states. It is not immediately clear if these are truly smallpox or mistaken diagnoses. By evening, laboratory confirmation of smallpox is obtained at CDC. Two cases in Montreal and one in London are also reported. CDC and health agencies now recognize that they are seeing a second generation of smallpox cases. It is presumed that the latest victims were infected by contact with those who attended the vice-president's speech, but a second bioterrorism attack cannot be immediately ruled out. CDC enlists additional epidemiologists from around the country to join teams tracking patients and their contacts.
Another 200 probable cases are reported during the day. CDC receives thousands of requests for vaccine from individual physicians and announces that vaccine will be distributed only through state health departments. Governors of a dozen states are calling the White House, demanding vaccine. One state attorney general announces a suit against the federal government to force release of vaccine for a large-scale vaccination campaign.
The federal government announces that 90% of available vaccine stocks will be distributed to affected states, but cautions that the available quantity of vaccine can cover only 15% of those states' populations. Governors are to determine their own state-specific priorities and mechanisms of vaccine distribution. Federal officials also announce an accelerated crash vaccine-production program that will reduce vaccine-manufacturing time to 24 months.
April 30
A well-known college athlete dies of hemorrhagic smallpox. The rumor is reported that he was the victim of a new biological attack using a different organism since he did not develop the rash associated with classic smallpox. Television commentators misinterpret technical statements from a health-care expert; the commentators report that the athlete died of hemorrhagic fever, and they read clinical descriptions of Ebola virus infection on the air.
The White House and CDC receive dozens of calls from furious governors, mayors, and health commissioners, demanding to know why they were not informed of additional bioterrorist attacks using Ebola. Nurses, doctors, and hospital-support personnel in health centers walk off the job. Thousands of people who attended college basketball games where the deceased athlete played call the health department and ask for treatment.
HHS issues a press release explaining that the athlete did not have Ebola virus. FBI affirms that there is no reason to believe that an attack using any hemorrhagic fever virus has occurred, but FBI refuses to rule out the possibility that there has been more than a single bioterrorist attack using smallpox.
April 31
The widely publicized death of the college basketball star, plus dramatic footage of young children covered with pox, drive thousands of people to emergency rooms and doctors' offices with requests for vaccination and evaluation of fever and other symptoms. This escalation in requests for evaluation and care hampers the ability of state health authorities and CDC to confirm the number of actual new cases.
May 1
The number of smallpox cases continues to grow. There are now >700 reported cases worldwide. In Northeast, the capacity of local hospitals to accommodate patients needing isolation has long been exceeded. Smallpox cases and suspected contacts are being isolated in the local armory and convention center, where volunteer physicians and nurses are providing care.
May 5
Epidemiologists are working around the clock to interview patients, trace the chain of infection, place contacts under surveillance, and isolate smallpox victims. The evidence continues to indicate that the vice-president's visit to Northeast was the occasion for the release, but some authorities remain concerned about multiple releases.
May 15-29
The third generation of the epidemic begins. Cases are reported in Northeast, parts of the country far beyond Northeast, and worldwide. The death rate remains 30%. Vaccine supplies are exhausted. Public concern is mounting rapidly. The president has declared states with the largest numbers of victims and people in quarantine to be disaster areas. Congress votes to release federal funds to pay for costs of quarantine. Over the next 2 weeks, 7,000 cases will have been reported.
May 30
The fourth generation of cases begins. By mid-June, 15,000 cases of smallpox will be reported in the United States. Twenty states report cases, as do four foreign countries. More than 2,000 will have died. The deceased include two members of the vice-president's staff and a secret service agent.
The city of Northeast, which is hardest hit by the epidemic, has experienced several outbreaks of civil unrest. The National Guard has been called in to help police keep order and to guard the facilities where smallpox cases and contacts are isolated. The mayor of Northeast is hospitalized with a heart attack.
Conclusions
The rate of development of new smallpox cases reported worldwide now appears to be stabilizing and perhaps subsiding. Vaccination of contacts has undoubtedly been of benefit. Perhaps more important is the seasonal decrease in the spread of virus as warmer weather returns.
Many business conventions scheduled to convene in Northeast during the early summer are canceled. Tourist trade, a major source of state income, is at a standstill. Many small businesses in the city have failed because suppliers and customers are reluctant to visit the area. Attendance at theaters and sports events is down markedly. In several states, public schools are dismissed 1 month early, in part because parents, fearful of contagion, are keeping their children home, and partly because teachers are refusing to come to work. Across the country, people refuse to serve on juries or attend public meetings for fear of contracting smallpox. In hospitals and HMOs where staff have not been vaccinated, health-care personnel have staged protests, and some have walked off the job.
The exponential increase in cases around the globe has caused some governments to institute strict, harshly enforced isolation and quarantine procedures. Human rights organizations report numerous cases of smallpox patients being abandoned to die or of recovering patients being denied housing and food.
Domestic and international travel is greatly reduced. Travelers avoid countries known to have smallpox. Some countries refuse to admit U.S. citizens without proof of recent smallpox vaccination. Others have imposed 14-day quarantines on all persons entering the country from abroad. A lucrative black market in falsified vaccination certificates has sprung up.
Congress has begun oversight investigations into the epidemic. A congressman accuses the U.S. Food and Drug Administration of deliberately obstructing the development of smallpox vaccine and vows to hold hearings into the matter. Congressional investigations of what FBI knew, when they knew it, and whom they talked with, are ongoing. Multiple lawsuits have been filed on behalf of and against HMOs, hospitals, and state and federal governments. Several large HMOs refuse to pay states for costs associated with caring for patients in isolation wards and quarantine facilities. The states with largest numbers of cases have spent millions of dollars on the epidemic, including establishing quarantine operations, paying for added public health personnel, and overtime pay for police.
In the United States, periodic rumors of miracle treatments, many fueled by the media, provoke ardent demands on a beleaguered health-care system. Since vaccine supplies were depleted, many people seeking protection have turned to ancient techniques. Some physicians are practicing arm-to-arm transfer of vaccinia, with a few attempting immunization with inoculation of smallpox virus from pustules.
Smallpox continues to spread in many parts of the world, echoing its formerly endemic character. Without vaccine, the only control method is isolation, which hinders, but cannot halt, the spread of the disease. By year's end, endemic smallpox is reestablished in 14 countries. The World Health Assembly schedules a debate on reenacting a global smallpox eradication campaign.
Dr. O'Toole is a senior fellow at the Johns Hopkins University Center for Civilian Biodefense Studies. The Center, sponsored by the Hopkins Schools of Public Health and Medicine, is dedicated to informing policy decisions and promoting practices that would help prevent the use of biological weapons.
Address for correspondence: Tara O'Toole, Johns Hopkins Center for Civilian Biodefense Studies, Candler Building, Suite 850, 111 Market Place, Baltimore, MD 21202, USA; fax: 410-223-1665; e-mail: [email protected].
=============================================================
87.) Smallpox: An attack scenario.
=============================================================
Emerg Infect Dis 1999 Jul-Aug;5(4):540-6
Comment in:
Emerg Infect Dis. 1999 Nov-Dec;5(6):842
Emerg Infect Dis. 2000 Jul-Aug;6(4):433-4
Tara O'Toole
Johns Hopkins School of Public Health, Baltimore, Maryland, USA
Smallpox virus, which is among the most dangerous organisms that might be used by bioterrorists, is not widely available. The international black market trade in weapons of mass destruction is probably the only means of acquiring the virus. Thus, only a terrorist supported by the resources of a rogue state would be able to procure and deploy smallpox. An attack using the virus would involve relatively sophisticated strategies and would deliberately seek to sow public panic, disrupt and discredit official institutions, and shake public confidence in government.
The following scenario is intended to provoke thought and dialogue that might illuminate the uncertainties and challenges of bioterrorism and stimulate review of institutional capacities for rapid communication and coordinated action in the wake of an attack.
Capacity To Detect a Bioterrorist Attack and To Diagnose an Unusual Disease
April 1
The vice-president visits Northeast, a city of 2.5 million. His itinerary includes an awards ceremony, an appearance at a local magnet school, and a major speech at the local university. A crowd of 1,000 people, including students, is gathered in the university auditorium. Hundreds more wait outside, where the vice-president stops to shake hands and respond to queries from the media.
The Federal Bureau of Investigation (FBI) has information suggesting a possible threat against the vice-president from a terrorist group with suspected links to a rogue state. The group is known to have made inquiries about acquiring biological pathogens, including smallpox, and is suspected of having procured aerosolization equipment. FBI decides its information is too vague and too sensitive to pass on to the Department of Health and Human Services, local law enforcement authorities, or the state health department.
April 8
FBI informants report rumors that something happened while the vice-president was in Northeast.
April 12
A 20-year-old university student goes to the university hospital emergency room with fever and severe muscle aches. She is pale, has a temperature of 103°F, and is slightly leukopenic, but the physical exam and laboratory results are otherwise normal. She is presumed to have a viral infection and is sent home with instructions to drink fluids and take aspirin or ibuprofen for muscle aches. Later that day, a 40-year-old electrician arrives at the emergency room with severe lower backache, headache, shaking chills, and vomiting. He appears pale and has a temperature of 102°F and a pale erythematous rash on the face. The patient is a native of Puerto Rico, where he visited 10 days earlier. A diagnosis of dengue fever is considered, and the patient is discharged with ibuprofen and instructions to drink fluids.
April 13
Over the course of the day, four young adults in their twenties come to the university hospital emergency room with influenzalike symptoms and are sent home.
April 14
The female student returns to the emergency room after collapsing in class. She now has a red, vesicular rash on the face and arms and appears acutely ill. Her temperature is 102°F; her blood pressure is normal. She is admitted to an isolation room with presumptive diagnosis of adult chickenpox. She has had no contact with others known to have chickenpox.
April 15
The electrician first seen on April 12 returns to the emergency room by ambulance. He too has a vesicular rash and appears very ill. He is also admitted to an isolation room with presumptive diagnosis of chickenpox.
That evening at 6 p.m. the infectious disease consultant and the hospital epidemiologist meet on the elevator. The infectious disease specialist has just finished examining the student and the electrician, both of whom have vesicular rash on the face, arms, hands, and feet. The skin lesions are evolving in phase. The possibility of smallpox is raised. The infectious disease specialist takes a swab specimen from the electrician's skin lesions, sends it to the laboratory, and requests that it be examined by electron microscopy by an experienced technician. The doctor assures the technician that he will be vaccinated if the specimen shows smallpox. At 7:00 p.m., electron microscopy shows an orthopoxvirus consistent with variola—the smallpox virus.
At 7:15 p.m. the hospital epidemiologist declares a contagious disease emergency. The two patients are moved to negative-pressure rooms with HEPA filters. Visitors and hospital staff not already caring for and in contact with patients are forbidden to enter the floor. Infection-control nurses begin interviewing staff to determine who has been in face-to-face contact with the patients during initial emergency room visits and admission. The hospital epidemiologist calls the chair of the department of medicine and the hospital vice-president for medical affairs.
Within 45 minutes the chair of the department of medicine and the president of the hospital are meeting with the infectious disease physician, the hospital epidemiologist, the hospital vice-president for public relations, and the hospital's general counsel. The city and state health commissioners join the meeting by phone. The need to vaccinate and isolate all contacts of the patients is recognized and discussed. It is decided to secure the hospital. No one is allowed to leave until all persons are identified so that they can be vaccinated as soon as vaccine can be obtained from the Centers for Disease Control and Prevention (CDC). The possibility of identifying and vaccinating other patient contacts (e.g., family members not now in the hospital) is discussed, but no decisions are made because the hospital's legal authority for doing this is unclear.
Half an hour later, the state health commissioner calls FBI. He also contacts CDC to request that smallpox vaccine be released for hospital staff and patient contacts. Because vaccine supplies are limited, CDC requests that the diagnosis of smallpox first be confirmed at CDC. CDC calls FBI and arranges to fly a three-person Epidemic Intelligence Service team to Northeast for assistance.
By 9:30 p.m., an FBI special agent arrives at the hospital, secures biological samples taken from the patients, and drives them to Andrews Air Force Base, where a military aircraft flies the samples to CDC's Biosafety Level 4 laboratory in Atlanta, Georgia. FBI requests that city police be called to help maintain order and ensure that no patients, staff, or visitors leave the hospital until all occupants have been identified and their addresses have been recorded. More FBI agents and city police arrive on the hospital grounds.
Hospital visitors are confused and angered by police refusal to allow anyone to leave the hospital. No explanation is given for the containment to staff, visitors, or the police. Ambulances are rerouted to other hospitals. The rumor that smallpox has broken out rapidly spreads through the building, as do rumors that a terrorist wanted by FBI is in the building. A fight erupts between people trying to leave the facility and the police. Three people are injured and sent to the emergency room. More police and FBI agents arrive and surround the building.
The local television networks report the scene outside the hospital on the late night news. The hospital public relations representative explains that the lock-in is temporary and intended only to gather names and addresses so that people can be contacted and treated if a suspected, but unnamed, contagious disease is confirmed. CNN arrives and demands access to the hospital and affected patients. Rumors about what the contagious disease might be include Hong Kong flu, meningitis, Ebola virus, smallpox, and measles.
The mayor and state attorney general's office are contacted by the health commissioner. There is a phone discussion with the hospital's general counsel and epidemiologist about the right to impose quarantine. Visitors, nonessential personnel, and new patients are blocked from entering the hospital, but visitors already in the building are allowed to leave after their names and addresses are recorded.
FBI, however, is reluctant to allow anyone to leave the building. This provokes a lengthy exchange among the FBI agent-in-charge, the city police chief, and hospital administrators and attorneys. The dispute is resolved after a series of phone calls between FBI headquarters and the state attorney general's office.
Early Response
11:30 p.m.
The specimen arrives at CDC. At midnight, the diagnosis of smallpox is confirmed. A phone conference with hospital staff, the city police chief, the state health commissioner, the state attorney general, the governor, CDC, FBI, an assistant secretary of the Health and Human Service (HHS), and staff from the National Security Council and the White House (32 people in all) focuses on whether and how to release the information to the media. The mayor and the governor will go on television in the morning with the health commissioner. The FBI director will also make a statement. The president will address the country at noon.
CDC makes arrangements to release smallpox vaccine early the next morning for use by patient contacts and the health-care teams caring for hospitalized victims.
April 16
Morning conference calls between CDC, FBI, HHS, the National Security Council, and state health authorities are set up. Federal officials now assume that a bioterrorist attack has occurred in Northeast. There is concern that other attacks might also have taken place but not yet come to light or that further attacks might be imminent.
A representative from the counterterrorism office of the National Security Council asks if it is necessary or desirable to attempt a complete quarantine of Northeast, including closure of the city airport and a ban on rail traffic leaving from or stopping in the city. The group agrees that such a step is neither feasible nor warranted. A heated debate follows about the advisability of vaccinating all hospital staff and visitors at all facilities where a single case of smallpox is clinically suspected. The state health commissioner presses for enough vaccine for the entire city of Northeast.
FBI and CDC are reluctant to begin mass vaccination until the dimensions of the outbreak are better understood. It is decided to vaccinate all hospital staff and any visitors to the floor where the patients were located. All direct contacts of the patients will also be vaccinated. By the end of the long phone conference, the decision is made to vaccinate all health-care personnel, first responders, police, and firefighters in any city with confirmed cases of smallpox.
CDC Epidemic Intelligence Service officers arrive in Northeast to assist the state epidemiologist, who is establishing a statewide surveillance and case investigation system. Efforts begin to develop a registry of all face-to-face contacts of smallpox patients and to monitor, daily, all contacts for fever. Anyone who has fever >101°F is to be isolated, at home if possible, and be followed for rash.
The state health department activates a prearranged phone tree to query all hospitals and walk-in clinics in the state about similar cases and counsels immediate isolation of all suspected patients.
An additional eight admissions for fever and vesicular rash are discovered. All patients are extremely ill; two are delirious. The university hospital emergency room records are searched, and staff attempt to contact all patients who had fever during the previous week. Three more probable smallpox cases are discovered. Telephone follow-up reveals that one has been admitted to another hospital out of state.
CDC and state health officials discuss possible strategies for managing the epidemic if there is insufficient vaccine for all patient contacts, as seems likely. Home isolation of nonvaccinated patient contacts is considered, but the legal authorities, practical logistics, and ethical implications of such a strategy remain unclear and unresolved.
After discussion among state health authorities and university hospital staff, it is decided that the university will serve as the city's smallpox hospital and will accept transfers of smallpox patients now hospitalized at other facilities in the state. Other hospitals will refer patients to the university hospital or to the state armory but will not admit patients with suspected smallpox. Physicians will be urged to avoid seeking admission for most smallpox patients and to care for patients in their homes.
Arrangements are made by the state health commissioner to activate a state disaster plan, which establishes the armory as an emergency hospital for the quarantine of smallpox patients, in case the number of smallpox patients exceeds hospital isolation capabilities.
Quarantine and Vaccination
During the morning interagency phone conference, Department of Justice representatives raise questions about potential legal liabilities associated with adverse vaccine effects. The questions remain unresolved, but vaccination will proceed.
On the evening of April 16, the president goes on television to inform the nation of the bioterrorist attack by unknown terrorists, vows that the assailants will be identified and brought to justice, and urges calm and cooperation with health authorities.
The initial epidemiologic evidence and FBI information suggest that the smallpox release likely occurred during the vice-president's January speech at the university in Northeast. Efforts are begun to identify and vaccinate everyone who attended the speech. Additional health department personnel are detailed to help in the epidemiologic investigation. Media reports say that the government does not know how many people are sick or how widespread the outbreak might be.
By evening, 35 more cases are identified in eight emergency rooms and clinics around the city; 10 cases are reported in an adjoining state. CDC alerts all state health departments to be on alert for possible smallpox; CDC also urges prompt and strict isolation measures and instructs states to send specimens from suspected patients to its headquarters in Atlanta for definitive laboratory diagnosis.
April 17
In Northeast, 10,000 residents are vaccinated by the city and state health departments with assistance from volunteer physicians and nurses. Vaccination of the entire university student body, faculty, and staff is discussed and rejected by federal officials for fear that vaccine supplies will be needed for contacts of confirmed cases. State health officials continue to press for a statewide vaccination effort. Unions representing nurses and other health-care workers call for vaccination of all employees whose jobs involve direct patient contact.
April 18
An additional 20,000 residents of Northeast are vaccinated.
April 19
CDC and the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) determine that the infecting strain of smallpox was not bioengineered. The genomic sequence is entirely typical of known smallpox strains.
The student with the first diagnosed case dies. Ten more smallpox cases have been identified, bringing the number of confirmed cases to 50. The patients are located in four states, all in the mid-Atlantic area. Suspected cases are identified in five other states.
April 20
Governors of affected and unaffected states press, both behind the scenes and publicly, for emergency vaccine stocks to be distributed to states so that immediate action can be taken should an outbreak occur.
At the close of day 4 of the vaccination campaign, 80,000 have been vaccinated.
April 22-27
No new cases of smallpox with onset after April 19 have been confirmed, although many suspected cases with fever and rash due to other causes are being seen. In the states reporting confirmed smallpox cases, thousands of people are seeking medical care because of worrisome symptoms. CDC and state health authorities decide to issue a recommendation that patients with fever who cannot be definitively diagnosed be strictly quarantined and observed until the fever subsides. CDC and state health departments are flooded with calls from health-care providers seeking guidance on isolation procedures.
Some hospitals and health maintenance organizations (HMOs) complain to HHS that they cannot afford to isolate the many patients with fever and rash at their facilities and demand that the government pay quarantine costs. State health departments are similarly worried about the costs of quarantine.
Local media report an outbreak of sick children with rash in an area elementary school. It is unclear whether the illness is chickenpox or smallpox. Television stations show film of parents arriving at school in midday to remove children from classrooms. A college basketball star is rushed to hospital by ambulance with an unknown illness. Local television reports that the athlete has high fever but no rash. Both stories are covered on the national evening news.
April 28
Smallpox is diagnosed in two young children in Megalopolis, a large city in another state. FBI and the National Security Council worry that these cases might signal another attack since the children have had no discernible contact with a smallpox patient or contacts. The possibility that there has been a new attack is weighed against the possibility that the children were infected by a contact of one of the first wave of patients who was missed in the epidemiologic investigation.
Members of the state congressional delegation demand that the federal government implement a massive citywide vaccination program. CDC notes that a Megalopolis-wide vaccination program would deplete the entire civilian vaccine supply.
The media report that the president, vice-president, cabinet representatives, and prominent members of Congress have been vaccinated, and the military has already begun to vaccinate the troops in affected states and Washington, D.C.
The Epidemic Expands
April 29
Over the course of the day, CDC receives reports of an additional 100 new cases of potential smallpox. Sixty of these are in the original state. The others are scattered over eight states. It is not immediately clear if these are truly smallpox or mistaken diagnoses. By evening, laboratory confirmation of smallpox is obtained at CDC. Two cases in Montreal and one in London are also reported. CDC and health agencies now recognize that they are seeing a second generation of smallpox cases. It is presumed that the latest victims were infected by contact with those who attended the vice-president's speech, but a second bioterrorism attack cannot be immediately ruled out. CDC enlists additional epidemiologists from around the country to join teams tracking patients and their contacts.
Another 200 probable cases are reported during the day. CDC receives thousands of requests for vaccine from individual physicians and announces that vaccine will be distributed only through state health departments. Governors of a dozen states are calling the White House, demanding vaccine. One state attorney general announces a suit against the federal government to force release of vaccine for a large-scale vaccination campaign.
The federal government announces that 90% of available vaccine stocks will be distributed to affected states, but cautions that the available quantity of vaccine can cover only 15% of those states' populations. Governors are to determine their own state-specific priorities and mechanisms of vaccine distribution. Federal officials also announce an accelerated crash vaccine-production program that will reduce vaccine-manufacturing time to 24 months.
April 30
A well-known college athlete dies of hemorrhagic smallpox. The rumor is reported that he was the victim of a new biological attack using a different organism since he did not develop the rash associated with classic smallpox. Television commentators misinterpret technical statements from a health-care expert; the commentators report that the athlete died of hemorrhagic fever, and they read clinical descriptions of Ebola virus infection on the air.
The White House and CDC receive dozens of calls from furious governors, mayors, and health commissioners, demanding to know why they were not informed of additional bioterrorist attacks using Ebola. Nurses, doctors, and hospital-support personnel in health centers walk off the job. Thousands of people who attended college basketball games where the deceased athlete played call the health department and ask for treatment.
HHS issues a press release explaining that the athlete did not have Ebola virus. FBI affirms that there is no reason to believe that an attack using any hemorrhagic fever virus has occurred, but FBI refuses to rule out the possibility that there has been more than a single bioterrorist attack using smallpox.
April 31
The widely publicized death of the college basketball star, plus dramatic footage of young children covered with pox, drive thousands of people to emergency rooms and doctors' offices with requests for vaccination and evaluation of fever and other symptoms. This escalation in requests for evaluation and care hampers the ability of state health authorities and CDC to confirm the number of actual new cases.
May 1
The number of smallpox cases continues to grow. There are now >700 reported cases worldwide. In Northeast, the capacity of local hospitals to accommodate patients needing isolation has long been exceeded. Smallpox cases and suspected contacts are being isolated in the local armory and convention center, where volunteer physicians and nurses are providing care.
May 5
Epidemiologists are working around the clock to interview patients, trace the chain of infection, place contacts under surveillance, and isolate smallpox victims. The evidence continues to indicate that the vice-president's visit to Northeast was the occasion for the release, but some authorities remain concerned about multiple releases.
May 15-29
The third generation of the epidemic begins. Cases are reported in Northeast, parts of the country far beyond Northeast, and worldwide. The death rate remains 30%. Vaccine supplies are exhausted. Public concern is mounting rapidly. The president has declared states with the largest numbers of victims and people in quarantine to be disaster areas. Congress votes to release federal funds to pay for costs of quarantine. Over the next 2 weeks, 7,000 cases will have been reported.
May 30
The fourth generation of cases begins. By mid-June, 15,000 cases of smallpox will be reported in the United States. Twenty states report cases, as do four foreign countries. More than 2,000 will have died. The deceased include two members of the vice-president's staff and a secret service agent.
The city of Northeast, which is hardest hit by the epidemic, has experienced several outbreaks of civil unrest. The National Guard has been called in to help police keep order and to guard the facilities where smallpox cases and contacts are isolated. The mayor of Northeast is hospitalized with a heart attack.
Conclusions
The rate of development of new smallpox cases reported worldwide now appears to be stabilizing and perhaps subsiding. Vaccination of contacts has undoubtedly been of benefit. Perhaps more important is the seasonal decrease in the spread of virus as warmer weather returns.
Many business conventions scheduled to convene in Northeast during the early summer are canceled. Tourist trade, a major source of state income, is at a standstill. Many small businesses in the city have failed because suppliers and customers are reluctant to visit the area. Attendance at theaters and sports events is down markedly. In several states, public schools are dismissed 1 month early, in part because parents, fearful of contagion, are keeping their children home, and partly because teachers are refusing to come to work. Across the country, people refuse to serve on juries or attend public meetings for fear of contracting smallpox. In hospitals and HMOs where staff have not been vaccinated, health-care personnel have staged protests, and some have walked off the job.
The exponential increase in cases around the globe has caused some governments to institute strict, harshly enforced isolation and quarantine procedures. Human rights organizations report numerous cases of smallpox patients being abandoned to die or of recovering patients being denied housing and food.
Domestic and international travel is greatly reduced. Travelers avoid countries known to have smallpox. Some countries refuse to admit U.S. citizens without proof of recent smallpox vaccination. Others have imposed 14-day quarantines on all persons entering the country from abroad. A lucrative black market in falsified vaccination certificates has sprung up.
Congress has begun oversight investigations into the epidemic. A congressman accuses the U.S. Food and Drug Administration of deliberately obstructing the development of smallpox vaccine and vows to hold hearings into the matter. Congressional investigations of what FBI knew, when they knew it, and whom they talked with, are ongoing. Multiple lawsuits have been filed on behalf of and against HMOs, hospitals, and state and federal governments. Several large HMOs refuse to pay states for costs associated with caring for patients in isolation wards and quarantine facilities. The states with largest numbers of cases have spent millions of dollars on the epidemic, including establishing quarantine operations, paying for added public health personnel, and overtime pay for police.
In the United States, periodic rumors of miracle treatments, many fueled by the media, provoke ardent demands on a beleaguered health-care system. Since vaccine supplies were depleted, many people seeking protection have turned to ancient techniques. Some physicians are practicing arm-to-arm transfer of vaccinia, with a few attempting immunization with inoculation of smallpox virus from pustules.
Smallpox continues to spread in many parts of the world, echoing its formerly endemic character. Without vaccine, the only control method is isolation, which hinders, but cannot halt, the spread of the disease. By year's end, endemic smallpox is reestablished in 14 countries. The World Health Assembly schedules a debate on reenacting a global smallpox eradication campaign.
Dr. O'Toole is a senior fellow at the Johns Hopkins University Center for Civilian Biodefense Studies. The Center, sponsored by the Hopkins Schools of Public Health and Medicine, is dedicated to informing policy decisions and promoting practices that would help prevent the use of biological weapons.
Address for correspondence: Tara O'Toole, Johns Hopkins Center for Civilian Biodefense Studies, Candler Building, Suite 850, 111 Market Place, Baltimore, MD 21202, USA; fax: 410-223-1665; e-mail: [email protected].
==================================================================
DATA-MEDICOS/DERMAGIC-EXPRESS No 3-(101) 30/06/2.001 DR. JOSE
LAPENTA R.
===================================================================
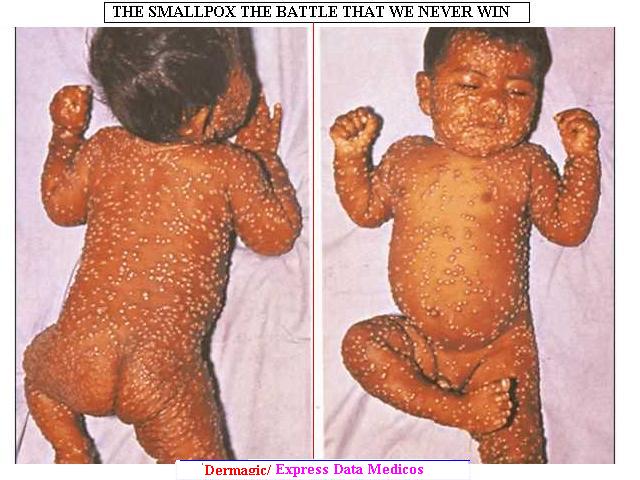
|